Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.
The COVID-19 pandemic may lead to cardiovascular pathological manifestations, necessitating a high level of vigilance for all affected patients. This issue's highlights focus on elucidating the pathophysiology of COVID-19 infection and its impact on cardiovascular patients to improve outcomes for those affected.
Issue release: 31 December 2021
Objective: To investigate the effect of optimized left atrioventricular conduction time (Lavi) on hemodynamics and prognosis of patients with third degree atrioventricular block implanted with dual chamber pacemakers. Methods: 120 patients with third degree atrioventricular block implanted with dual chamber pacemaker were randomly divided into Lavi optimized group and non optimized group. Oesophageal electrocardiography was performed 3 months after pacemaker implantation (observation base point). The atrial conduction time (IACT) and interventricular conduction time (IVCT) of the two groups were measured and the Lavi under the default atrioventricular delay (AVD) state of the pacemaker was calculated. The optimization group then adjusted the AVD of the pacemaker under the guidance of echocardiography to obtain the optimal Lavi under the best mechanical synchronization state of the left atrioventricular. All patients were examined by echocardiography at 6, 12 and 18 months after operation. ECG conduction parameters, related clinical manifestations and prognostic indicators were observed, and the relationship between optimal Lavi and heart rate was analyzed. Results: a) In the optimization group, the average optimal Lavi was (130.8 ± 11.9) ms, which was longer than the default Lavi value (120.7 ± 18.7ms) (p < 0.05). b) In the optimization group, the optimal Lavi was negatively correlated with heart rate (r = −0.955, p < 0.05), heart rate <70 beats/min, and the optimal Lavi was 140 ms; the heart rate was 70~80 beats/min, and the optimal Lavi was 130ms; heart rate >80 beats/min, and the optimal Lavi is 120 ms. c). Optimization of Lavi could immediately improve e-peak deceleration time (EDT) and isovolumic relaxation time (IVRT) in the optimization group (p < 0.05). d) The left ventricular ejection fraction (LVEF), EDT and IVRT of the optimized group were better than those of the non optimized group at 6 months after operation (p < 0.05), and the left atrial volume index and e/e ‘(the ratio of early diastolic flow velocity of mitral orifice to early diastolic movement velocity of mitral annulus) were better than those of the non optimized group at 12 months after operation (p < 0.05). e) LVEF and EDT in the non optimized group decreased gradually during the follow-up period of 18 months (p < 0.05); IVRT and left atrial volume index increased gradually during the whole follow-up period (p < 0.05). E/e ‘in the optimization group increased gradually during the follow-up period (p < 0.05), while EDT decreased gradually during the follow-up period (p < 0.05). f) The cumulative incidence of new paroxysmal atrial fibrillation in the optimization group was significantly lower than that in the non optimization group (8.3% vs. 23.3%, p < 0.05). Conclusion optimization of Lavi can improve hemodynamics and reduce the incidence of atrial fibrillation in patients with third degree atrioventricular block implanted with dual chamber pacemakers.
Issue release: 31 December 2021
Objective: The statistical number of cases was 73 times. 66 patients entered the study, including 31 males and 35 females, aged from 17 to 86 years. Firstly, the accurate big data analysis was carried out on 66 cases of ambulatory ECG, and then the corresponding time that can be compared and analyzed before and after 24 h was determined through the time (T) RR interval scatter diagram. The changes of 24 h ECG scatter diagram were observed, and the total number of heart beats and the number of premature beats were counted by the scatter diagram technique, and then compared and analyzed according to the type of arrhythmia. Results: A frequent or occasional premature beats: 52 patients (59 times), 26 males and 26 females, aged (56.1 ± 15.4) years; the effective analysis duration was (22.40 ± 1.19) H. There was a significant correlation between the number of heart beats before and after treatment (r = 0.934, p = 0.000). b. Persistent arrhythmia: 4 cases of persistent atrial fibrillation (referred to as atrial fibrillation), 1 case of frequent atrial and ventricular concurrent arrhythmia, 2 males and 3 females, aged (68.4 ± 9.4) years; the effective analysis duration was (22.68 ± 0.74) H. The t-RR scatter plot and Lorenz RR scatter plot of these patients had self-similarity before and after 24 h. There was no significant difference in the total heart beat number before and after 24 h[(111796 ± 16439) vs (111262 ± 16421), p = 0.624], and the total heart beat number before and after 24 h was significantly correlated (r = 0.991, p = 0.001); the qualitative diagnosis of long interval in 3 patients with atrial fibrillation was consistent 24 hours before and after diagnosis. c. Paroxysmal arrhythmia: 9 cases, 3 cases of paroxysmal atrial flutter, 5 cases of paroxysmal atrial fibrillation, and 1 case of paroxysmal vertical separation of sinus node function. There were 3 males and 6 females. The age was (71.2 ± 12.7) years. The effective analysis duration was (22.67 ± 0.74) H. Conclusion: 24 h ambulatory ECG can meet the requirements for patients with frequent or occasional premature beats and persistent arrhythmias, while 48 h ambulatory ECG may be necessary for patients with paroxysmal arrhythmias.
Issue release: 31 December 2021
Objective: To compare the predictive value of CHADS2, CHA2DS2-VASc, ATRIA and R2-CHADS2 scores and left atrial thrombosis and/or spontaneous ultrasound in patients with non-valvular atrial fibrillation (AF) Methods patients with non-valvular atrial fibrillation who were hospitalized in the Department of Cardiology of Sun Yat Sen Memorial. Results: 564 patients were included. The age of patients was (61.1 ± 10.1) years old, of which 63.3% were men. Hypertension was the most common complication, which was found in 49.6% of patients. Patients were divided into thrombus group (n = 82) and non-thrombus group (n = 482) according to the presence of left atrial thrombus and/or spontaneous ultrasound development CHADS2 score in thrombotic group (1[0,2]) was higher than that in non-thrombotic group (1[0,1]) (P < 0.05), and CHA2DS2-VASc score in thrombotic group (2[1,3]) was higher than that in non-thrombotic group (2[1,2]) (P < 0.05) 11.06%, 13.39%, 26.58%, 18.52% and 16.67% of patients with CHADS2 score of 0, 1, 2, 3 and 4 had left atrial thrombus and/or spontaneous ultrasound (P fortrend = 0.016), and 11.06%, 13.39% and 23.68% of patients with low, medium and high risk had left atrial thrombus and/or spontaneous ultrasound (P fortrend = 0.004); 10.81%, 10.19%, 16.57%, 21.05%, 21.05%, 16.67%, 14.29% of patients with CHA2DS2-VASc score of 0, 1, 2, 3, 4, 5, 6 or above had left atrial thrombosis and/or spontaneous ultrasound development (P fortrend = 0.019), and 8.75%, 13.90% and 19.35% of patients with low, medium and high risk had left atrial thrombosis and/or spontaneous ultrasound development (P fortrend = 0.004); The area under the ROC curve of ATRIA score and R2-CHADS2 score was 0.562. The samples based on this study had no statistical significance in the diagnosis of left atrial thrombosis and/or spontaneous ultrasound (P > 0.05). Conclusion: CHADS2 score and CHA2DS2-VASc score have considerable and limited diagnostic value for left atrial thrombosis and/or spontaneous ultrasound in patients with non-valvular atrial fibrillation.
Issue release: 31 December 2021
Although ECG has been developed for a hundred years, the mechanism of T wave formation is unknown. The proposal of in vitro wedge-shaped model has greatly promoted the understanding of T-wave formation mechanism. By comparing the action potentials of epicardial cells, medial cells and endocardial cells in wedge-shaped ventricular mass with the T wave of body surface ECG, it was found that the T wave was mainly formed by the dispersion of transmural repolarization of ventricular muscle. However, in the subsequent in vivo experiments, electrophysiologists found that the formation of T wave was related to the dispersion of ventricular global repolarization, and the repolarization order of different parts of the three-dimensional global heart determined the polarity of T wave. In the real heart, the mechanism of T wave formation may be more complex, its repolarization gradient may include repolarization in each axis of the heart, and the polarity of T wave may also be the result of multiple factors.
Issue release: 31 December 2021
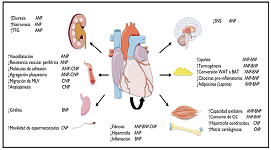
The current pandemic caused by the new coronavirus (SARS-CoV-2) has been the focus of worldwide health concern since its appearance. Its high transmissibility associated with the absence of an effective treatment implies a hard impact in the research area. Reports on atypical forms of presentation, associated risk factors and drugs tested to reduce morbidity and mortality saturate the media. The cardiological community is actively involved, since cardiovascular manifestations are frequent and varied, and an increased risk of poor outcome has been observed in individuals with previous cardiovascular disease. The aim of the review is to provide the available evidence on this topic, with the caveat that the information is dynamic.

Prof. Prakash Deedwania
University of California,
San Francisco, United States





 Open Access
Open Access