
Mathematical modeling of HIV/AIDS transmission dynamics: Mass rape and the use of post-exposure prophylaxis (PEP)
Vol 3, Issue 3, 2025
Download PDF
Abstract
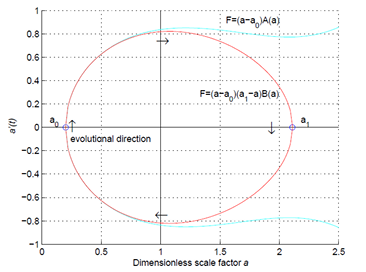
This study presents a deterministic mathematical model to investigate the transmission dynamics of HIV/AIDS, with a particular focus on mass rape as a significant driver of new infections and the mitigating effects of post-exposure prophylaxis (PEP) and antiretroviral (ARV) treatments. The model explicitly incorporates intensity of rape into the transmission framework and assesses the impact of PEP in reducing new HIV infections. Analytical results include the existence and uniqueness of positive solutions, equilibrium points, the basic reproduction number ( ), and global stability conditions for both disease-free and endemic equilibria. Numerical simulations are performed to support and illustrate the analytical findings. The results reveal a linear relationship between the incidences of rape and while showing an inverse relationship between PEP coverage and , indicating that timely and widespread PEP administration can significantly reduce HIV transmission, especially in regions affected by sexual violence. Furthermore, the study demonstrates that combined intervention strategies involving both PEP and ARV treatments produce synergistic effects, substantially suppressing HIV transmission. These findings emphasize the importance of integrated treatment strategies over isolated interventions. Despite the substantial impact of these interventions, the model suggests that the disease remains endemic under certain conditions. By explicitly integrating conflict-related factors, particularly mass rape and treatment disruption, this model provides a novel, evidence-based framework for informing policy in humanitarian emergencies. It enables global health actors to prioritize interventions and allocate limited resources more effectively.
Keywords
References
1. Daw MA, El‑Bouzedi HA, Ahmed MO. The impact of armed conflict on the prevalence and transmission dynamics of HIV infection in Libya. Front Public Health. 2022; 10: 779778. doi: 10.3389/fpubh.2022.779778
2. Kebede HK, Gesesew H, Ward P. Impact of armed conflicts on HIV treatment outcomes in sub‑Saharan Africa: protocol for a systematic review and meta‑analysis. BMJ Open. 2023; 13: e069308. doi: 10.1136/bmjopen-2022-069308
3. UNAIDS. Global HIV & AIDS Statistics – fact sheet. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 2 June 2025).
4. UNESCO. International Technical Guidance on Sexuality Education: An Evidence‑informed Approach. Revised ed. UNESCO, UNAIDS, UNFPA, UNICEF, UN Women & WHO; 2018. Available online: https://cdn.who.int/media/docs/default-source/reproductive-health/sexual-health/international-technical-guidance-on-sexuality-education.pdf (accessed on 2 June 2025).
5. United Nations Security Council. Resolution: Women and Peace and Security. United Nations; 2008. Available online: https://undocs.org/S/RES/1820(2008) (accessed on 2 June 2025).
6. Carpio MA. In the Democratic Republic of Congo, the double punishment of raped women (France). Available online: https://www.nationalgeographic.fr/histoire/en-republique-democratique-du-congo-la-double-peine-des-femmes-violees (accessed on 2 June 2025).
7. Anema A, Joffres MR, Mills E, Spigel PB. Widespread rape does not directly appear to increase the overall HIV prevalence in conflict‑affected countries: so now what? Emerging Themes in Epidemiology. 2008; 5: 11. doi: 10.1186/1742-7622-5-11
8. Supervie V, Halima Y, Blower S. Assessing the impact of mass rape on the incidence of HIV in conflict‑affected countries. AIDS. 2010; 24(18): 2841–2847. doi: 10.1097/QAD.0b013e32833fed78
9. Fisseha G, Gebrehiwot TG, Gebremichael MW, et al. War related sexual and gender‑based violence in Tigray, Northern Ethiopia: a community-based study. BMJ Global Health. 2023; 8(7): e010270. doi: 10.1136/bmjgh-2022-010270
10. Abrahams N, Mhlongo S, Dunkle K, et al. Increase in HIV incidence in women exposed to rape. AIDS. 2021; 35(4): 633–642. doi: 10.1097/QAD.0000000000002779
11. Mootz JJ, Odejimi OA, Bhattacharya A, et al. Transactional sex work and HIV among women in conflict‑affected Northeastern Uganda: a population-based study. Conflict and Health. 2022; 16: 8. doi: 10.1186/s13031-022-00441-5
12. Bennett BW, Marshall BDL, Gjelsvik A, et al. HIV incidence prior to, during, and after violent conflict in 36 Sub-Saharan African nations, 1990–2012: an ecological study. PLoS One. 2015; 10(11): e0142343. doi: 10.1371/journal.pone.0142343
13. Ba AT. Armed Conflicts, HIV Testing, HIV Prevalence, and High-Risk Sexual Behaviors: An Epidemiologic Analysis [PhD thesis]. Medical University of South Carolina; 2022. Available online: https://medica-musc.researchcommons.org/theses/704/ (accessed on 2 June 2025).
14. Ciswaka H, Oduoye MO, Masimango G, et al. Prevention and elimination efforts of HIV/AIDS caused by sexual violence against women in the Democratic Republic of the Congo: An editorial. International Journal of Gynecology & Obstetrics. 2024; 164(2): 385–386. doi: 10.1002/ijgo.15128
15. World Health Organization. WHO expands recommendation on oral pre-exposure prophylaxis of HIV infection (PrEP); 2015. Available online: https://www.paho.org/en/node/69890 (accessed on 2 June 2025).
16. Indonesian Ministry of Health. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection (SIHA),2024. Available online: https://siha.kemkes.go.id/portal/files_upload/9789241549684_eng.pdf (accessed on 2 June 2025).
17. Nsuami MUN, Witbooi PJ. A stochastic model for HIV with the use of PrEP. Journal of Mathematical Modeling. 2021; 9(4): 537–553. doi: 10.22124/jmm.2021.16870.1461
18. Peter OJ, Abidemi A, Fatmawati F, et al. Optimizing tuberculosis control: a comprehensive simulation of integrated interventions using a mathematical model. Mathematical Modelling and Numerical Simulation with Applications. 2024; 4(3): 238–255. doi: 10.53391/mmnsa.1461011
19. Ulfa B, Trisilowati T, WM K. Dynamical analysis of HIV/AIDS epidemic model with treatment. The Journal of Experimental Life Science. 2018; 8(1): 23–29. doi: 10.21776/ub.jels.2018.008.01.04
20. Ouaziz SI, El Khomssi M. Mathematical approaches to controlling COVID-19: optimal control and financial benefits. Mathematical Modelling and Numerical Simulation with Applications. 2024; 4(1): 1–36. doi: 10.53391/mmnsa.1373093
21. Cai L, Li X, Ghosh M, Guo B. Stability analysis of an HIV/AIDS epidemic model with treatment. Journal of Computational and Applied Mathematics. 2009; 229(1): 313–323. doi: 10.1016/j.cam.2008.10.067
22. Bashiru KA, Ojurongbe TA, Kolawole MK, et al. Stability analysis of HIV/AIDS epidemic model in the presence of vertical transmission and treatment. UNIOSUN Journal of Engineering and Environmental Sciences. 2023; 5(1). doi: 10.36108/ujees/3202.50.0141
23. Turan M, Sevinik Adıguzel R, Koc F. Stability analysis of an epidemic model with vaccination and time delay. Mathematical Methods in the Applied Sciences. 2023; 46(14): 14828–14840. doi: 10.1002/mma.9348
24. Kasia Ayele T, Doungmo Goufo EF, Mugisha S. Mathematical modeling of HIV/AIDS with optimal control: A case study in Ethiopia. Results in Physics. 2021; 26: 104263. doi: 10.1016/j.rinp.2021.104263
25. Mustapha UT, Ado A, Yusuf A, et al. Mathematical dynamics for HIV infections with public awareness and viral load detectability. Mathematical Modelling and Numerical Simulation with Applications. 2023; 3(3): 256–280. doi: 10.53391/mmnsa.1349472
26. Baba IA, Yusuf A, Al-Shomrani M. A mathematical model for studying rape and its possible mode of control. Results in Physics. 2021; 22: 103917. doi: 10.1016/j.rinp.2021.103917
27. Islam KN, Biswas MHA. Mathematical Assessment for the Dynamical Model of Sexual Violence of Women in Bangladesh. In: Proceedings of the International Conference on Industrial & Mechanical Engineering and Operations Management; 26-27 December 2020; Dhaka, Bangladesh.
28. Gurmu ED, Bole BK, Koya PR. Mathematical modelling of HIV/AIDS transmission dynamics with drug resistance compartment. American Journal of Applied Mathematics. 2020; 8(1): 34–45. doi: 10.11648/j.ajam.20200801.16
29. Van den Driessche P, Watmough J. Reproduction numbers and subthreshold endemic equilibria for compartmental models of disease transmission. Mathematical Biosciences. 2002; 180(1–2): 29–48. doi: 10.1016/S0025-5564(02)00108-6
30. Lu G, Dou L, Miao Y, Chen L. Co-dynamics of measles and hand-foot-mouth disease: Reproduction number and equilibrium analysis. Mathematics and Systems Science. 2025; 3(2): 1–20. doi: 10.54517/mss3359
31. Berman A, Plemmons RJ. Nonnegative Matrices in the Mathematical Sciences. SIAM; 1994. doi:10.1137/1.9781611971262
Supporting Agencies
Copyright (c) 2025 Abdelkadir Muzey Mohammed, Habtu Alemayehu Astbaha, Yohannes Yirga Kefela, Woldegebriel Assefa Woldegerima, Kiros Tedla Gebrehiwot

This work is licensed under a Creative Commons Attribution 4.0 International License.
Editor-in-Chief

Prof. Youssri Hassan Youssri
Cairo University, Egypt
Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.

.jpg)

.jpg)
