
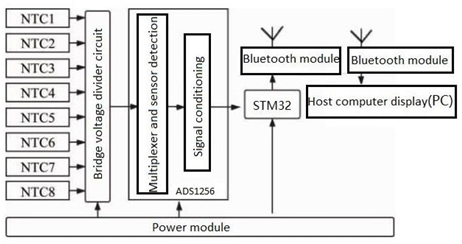
This paper delves deeply into the innovative realm of integrating human emotions with wearable technology. The primary focus is on the conceptualization and development of a kiss transfer device that harnesses the power of wearable technology to bridge the physical gap in human-human interactions. By investigating the intricate nuances of the human-human kissing process, the research seeks to replicate this intimate gesture through a technological medium. The paper not only elaborates on the anatomy, evolution, and hormonal dynamics of kissing but also underscores the transformative potential of wearable technology in capturing and transmitting these intimate moments. This exploration opens up new horizons for long-distance relationships, offering a tangible touchpoint that goes beyond traditional communication methods. Through this pioneering work, the research positions wearable technology as not just a tool for communication but as an extension of our human emotions and expressions.
Extra short implants in jaws with extreme vertical resorption: Case series
Vol 1, Issue 2, 2020
Download PDF
Abstract
Introduction: The use of in vitro implants can repair severe resorption. This sometimes requires the use of prostheses in the most extreme cases, when the proportion of crown implants is not ideal, to reach 2:1 or 3:1. Materials and methods: clinical analysis was carried out on implants with a residual of 5.5mm or less and more than 6 months. Chi square test was used for categorical variables and student t–test was used for continuous variables. Then, a linear fitting regression model is established. Results: Six patients received in vitro implantation. 21.2% of the patients in the study were male and 78.8% were female, with an average age of 57 years. The average crown planting ratio was 3.19 (+/–0.24). The average bone loss of the implant was 0.86mm (+/–0.33) in the near median position and 0.83mm (+/–0.47) in the anterior position. There was no statistically significant difference in the functional proportion of proximal and distal bone loss (P=0.224). Conclusion: According to the data provided in this study, even if the crown implant.
Keywords
References
- Chiapasco M, Ferrini F, Casentini P, et al. Dental implants placed in expanded narrow edentulous ridges with the extension crests device. A 1–3 year multicenter follow–up study. Clin Oral Impl Res 2006; 17(3): 265–272.
- Storgard S, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone–substitute materials. Jomi 2009; 24: 218–236.
- Blus C, Szmukler–Moncler S. Split–crest and immediate implant placement with ultra–sonic bone surgery: a 3–year life–table analysis with 230 treated sites. Clin Oral Impl Res 2006; 17(6): 700–707.
- Demarosi F, leghissa GC, Sardella A, et al. Local maxillary crest expansion and simultaneous implantation: case series. Journal Of Oral and Maxillofacial Surgery, 2009; 47(7): 535–540.
- Basa S, Varol A, Turker N. Alternative bone expansion technique for immediate placement of implants in the edentulous posterior mandibular ridge: a clinical report. Jomi 2004; 19(4): 554–558.
- Albrektsson T, Zarb G, Worthington P, et al. The long term efficacy of currently used dental immplants. A review and proposed criteria of success. Int J Oral Maxillofac Implants 1986; 1(1): 11–25.
- Ten Bruggenkate CM, van der Kwast WA, Osterbeek HS. Success criteria in oral implantology. A Review of the literature. Int J Oral Implantol 1990; 7(1): 45–51.
- Deporter D, Todescan R, Caudry S. Simplifying management of the posterior maxilla using short, porous–surfaced dental implants and simultaneous indirect sinus elevation. Int J Periodontics Restorative Dent 2000; 20(5): 476–485.
- Jain N, Gulati M, Garg M, et al. Short implants: new horizon in implant dentistry. J Clin Diagn Res 2016; 10(9): ZE14–ZE17.
- Lemos CA, Ferro–Alves ML, Okamoto R, et al. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and metaanalysis.J Dent 2016; 47: 8–17. doi: 10.1016/j.jdent.2016.01.005
- Anitua E, Alkhraisat MH, Orive G. Novel technique for the treatment of the severely atrophied posterior mandible. Int J Oral Maxillofac Implants 2013; 28(5): 1338–1346.
- Anitua E, Orive G, Aguirre JJ, et al. Five–year clinical evaluation of short dental implants placed in posterior areas: a retrospective study. J Periodontol 2008; 79(1): 42–48.
- Anitua E. The use of short and extra–short BTI implants in the daily clinical practice. JIACD 2010; 2(5): 19–29.
- Anitua E, Orive G. Short implants in maxillae and mandibles: a retrospective study with 1 to 8 years of follow–up. J Periodontol 2010; 81(6): 819–826.
- Anitua E, Alkhraist MH, Piñas L, et al. Implant survival and crestal bone loss around extra–short implants supporting a fixed denture: the effect of crown height space, crown–to–implant ratio, and off set placement of the prosthesis. Int J Oral Maxillofac Implants 2014; 29(3): 682–689.
- Anitua E, Piñas L, Begoña L, et al. Long–term retrospective evaluation of short implants in the posterior areas: clinical results after 10–12 years. J Clin Periodontol 2014; 41(4): 404–411.
- Anitua E, Alkhraisat MH, Piñas L, et al. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat 2015; 199: 9–15. doi: 10.1016/j.aanat.2014.02.005.
- Anitua E, Piñas L, Murias–Freijo A, et al. Rehabilitation of Atrophied Low–Density Posterior Maxilla by Implant–Supported Prosthesis. J Craniofac Surg 2016; 27(1): e1–2.
- Rokni S, Todescan R, Warson P, et al. An assessment of crown–to–root ratios with short sintered porous–surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants 2005; 20(1): 69–76.
- Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006; 21(2): 275–282.
- Birdi H, Schulte J, Kovacs A, et al. Crown–to–implant ratios of short–length implants. J Oral Implantol 2010; 36(6): 425–433.
- Nissan J, Ghelfan O, Gross O, et al. The effect of crown/implant ratio and crown height space on stress distribution in unsplinted implant supporting restorations. J Oral Maxillofac Surg 2011; 69(7): 1934–1939.
- Nissan J, Ghelfan O, Gross O, et al. The effect of splinting implant–supported restorations on stress distribution of different crown–implant ratios and crown height spaces. J Oral Maxillofac Surg 2011; 69(12): 2990–2994.
- Grossmann Y, Finger IM, Block MS. Indications for splinting implant restorations. J Oral Maxillofac Surg 2005; 63(11): 1642–1650.
Supporting Agencies
Copyright (c) 2020 Eduardo Anitua

This work is licensed under a Creative Commons Attribution 4.0 International License.

Prof. Zhen Cao
College of Information Science & Electronic Engineering, Zhejiang University
China, China
Processing Speed
-
-
-
- <5 days from submission to initial review decision;
- 62% acceptance rate
-
-
Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.





