
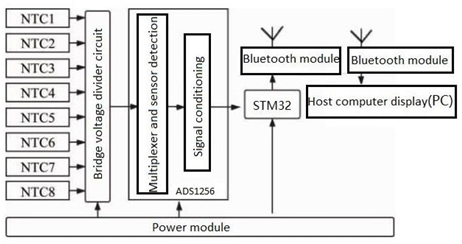
This paper delves deeply into the innovative realm of integrating human emotions with wearable technology. The primary focus is on the conceptualization and development of a kiss transfer device that harnesses the power of wearable technology to bridge the physical gap in human-human interactions. By investigating the intricate nuances of the human-human kissing process, the research seeks to replicate this intimate gesture through a technological medium. The paper not only elaborates on the anatomy, evolution, and hormonal dynamics of kissing but also underscores the transformative potential of wearable technology in capturing and transmitting these intimate moments. This exploration opens up new horizons for long-distance relationships, offering a tangible touchpoint that goes beyond traditional communication methods. Through this pioneering work, the research positions wearable technology as not just a tool for communication but as an extension of our human emotions and expressions.
Prevalence and characteristics of findings related implant in panoramic x-rays
Vol 1, Issue 2, 2020
Download PDF
Abstract
Introduction: In Colombia, the latest oral health study shows that about 70% of the population suffer from partial edentulism, while 5.2% lose all teeth between the ages of 65 and 79. Implant rehabilitation is an increasingly and widely used option, which requires clinical and X-ray follow-up. Panoramic X-ray examination is a low-cost option. In this case, the area of bone loss, the middle and distal angle of the implant, the relationship with the anatomical structure and the related lesions of periimplant inflammation can be observed. Data on X-ray findings associated with dental implants need to be reported and analyzed to determine risk factors for success in patients using these implants. Objective: To determine the prevalence and characteristics of findings related to osseointegrated implants in panoramic X-ray films. Methods: Descriptive cross-sectional observation was used to select 10,000 digital panoramic photos from the radiation center in Bogota, Colombia, of which 543 were related to the presence of implants. The position, angle and distance from adjacent structures of each implant were evaluated using program ClínicalView® (Orthopantomograph OP200D, Instrumentarium, USA). Result: The X-ray frequency of implants was 5.43%. There were 1,791 implants, with an average of 3.2 X-rays per time. They have a higher proportion in the maxilla and are located on the crest at an angle of 10.3 degrees. 32% of patients had implant/tooth or implant/implant distance below the optimal value. 40.9% of the patients were repaired, and 1.2% of the patients had periodontitis. Conclusion: The high proportion of modified implants has a risk factor that affects their long-term survival, whether due to angle, ridge or ridge location, adjacent teeth or other implants, or because they are irreparable.
Keywords
References
- Russell SL, Gordon S, Lukacs JR, et al. Sex/Gender differences in tooth loss and edentulism: Historical perspectives, biological factors, and sociologic reasons. Dental Clinics 2013; 57(2): 317–337.
- IV National Study of Oral Health (ENSAB IV) Bogota: Ministry of Health of Colombia. Available at: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENSABIV-Situacion-Bucal-Actual.pdf. (Accessed Oct. 20, 2016).
- Chugh NK, Bhattacharyya J, Das S, et al. Use of digital panoramic radiology in presurgical implant treatment planning to accurately assess bone density. The Journal of Prosthetic Dentistry 2016; 116(2): 200–205.
- Gutmacher Z, Machtei EE, Hirsh I, et al. A comparative study on the use of digital panoramic and periapical radiographs to assess proximal bone height around dental implants. Quintessence International 2016; 47(5): 441–446.
- Cortes ARG, Eimar H, Barbosa J S, et al. Sensitivity and specificity of radiographic methods for predicting insertion torque of dental implants. Journal of Periodontology 2015; 86(5): 646–655.
- Machtei EE, Oettinger-Barak O, Horwitz J. Axial relationship between dental implants and teeth/implants: a radiographic study. Journal of Oral Implantology 2014; 40(4): 425–431.
- Saulacic N, Abboud M, Pohl Y, et al. Implant-supported mandibular overdentures and cortical bone formation: clinical and radiographic results. Implant Dentistry 2014; 23(1): 85–91.
- Caubet J, Heras I, Sanchez J, et al. Management of anteroposterior bone defects in aestethic restoration of the front teeth. Revista Espanola deCirugia Oral y Maxilofacial 2009; 31(2): 81–97.
- Aradya A, Kumar UK, Chowdhary R. Influence of different abutment diameter of implants on the peri-implant stress in the crestal bone: A Three-dimensional finite element analysis-In vitro study. Indian Journal of Dental Research 2016; 27(1): 78–85.
- Behnaz E, Ramin M, Abbasi S, et al. The effect of implant angulation and splinting on stress distribution in implant body and supporting bone: A finite element analysis. European Journal of Dentistry 2015; 9(03): 311–318.
- Ishak MI, Kadir MRA, Sulaiman E, et al. Finite element analysis of different surgical approaches in various occlusal loading locations for zygomatic implant placement for the treatment of atrophic maxillae. International Journal of Oral and Maxillofacial Surgery 2012; 41(9): 1077–1089.
- Sáenz Guzmán M. Criteria for success and failure of osseointegrated dental implants. Acta OdontológicaVenezolana 2013; 51(2): 150–158.
- Negri M, Galli C, Smerieri A, et al. (2014) The effect of age, gender, and insertion site on marginal bone loss around endosseous implants: Results from a 3-year trial with premium implant system. BioMed Research International 2014.
- Pinchi V, Varvara G, Pradella F, et al. Analysis of professional malpractice claims in implant dentistry in Italy from insurance company technical reports, 2006 to 2010. International Journal of Oral & Maxillofacial Implants 2014; 29(5): 1177–1184.
- Lee YK, Kim JW, Baek SH, et al. Root and bone response to the proximity of a mini-implant under orthodontic loading. Angle Orthodontist 2010; 80(3): 452–458.
- Danza M, Zollino I, Avantaggiato A, et al. Distance between implants has a potential impact of crestal bone resorption. The Saudi Dental Journal 2011; 23(3): 129–133.
- Jo DW, Yi YJ, Kwon MJ, et al. Correlation between interimplant distance and crestal bone loss in internal connection implants with platform switching. International Journal of Oral & Maxillofacial Implants 2014; 29(2): 296–302.
- Siadat H, Panjnoosh M, Alikhasi M, et al. Does implant staging choice affect crestal bone loss? Journal of Oral and Maxillofacial Surgery 2012; 70(2): 307–313.
- Misch CE, Perel ML, Wang HL, et al. Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) pisa consensus conference. Implant Dentistry 2008; 17(1): 5–15.
- Al Amri MD. Influence of interimplant distance on the crestal bone height around dental implants: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry 2016; 115(3): 278–282.
- Duque AD, Aristizabal AG, Londono S, et al. Prevalence of peri-implant disease on platform switching implants: a cross-sectional pilot study. Brazilian Oral Research 2016; 30(1).
- Van Eekeren P, Tahmaseb A, Wismeijer D. Crestal bone changes in macrogeometrically similar implants with the implant-abutment connection at the crestal bone level or 2.5 mm above: a prospective randomized clinical trial. Clinical Oral Implants Research 2015; 27(12): 1479–1484.
- Trullenque-Eriksson A, Moya BG. Retrospective long-term evaluation of dental implants in totally and partially edentulous patients: part II: periimplant disease. Implant Dentistry 2015; 24(2): 217–221.
- De Bruyn H, Vandeweghe S, Ruyffelaert C, et al. Radiographic evaluation of modern oral implants with emphasis on crestal bone level and relevance to peri-implant health. Periodontology 2000, 2013; 62(1): 256–270.
- Pabst AM, Walter C, Ehbauer S, et al. Analysis of implant-failure predictors in the posterior maxilla: a retrospective study of 1395 implants. Journal of Cranio-Maxillofacial Surgery 2015; 43(3): 414–420.
Supporting Agencies
Copyright (c) 2020 Silvia Barrientos Sánchez, Adriana Rodríguez Ciodaro, David Martínez Laverde, Alejandro Curan Cantoral

This work is licensed under a Creative Commons Attribution 4.0 International License.

Prof. Zhen Cao
College of Information Science & Electronic Engineering, Zhejiang University
China, China
Processing Speed
-
-
-
- <5 days from submission to initial review decision;
- 62% acceptance rate
-
-
Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.





