Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.
The research progress of microparticles (extracellular vesicles) in the field of cardiovascular surgery
Vol 1, Issue 1, 2020
Download PDF
Abstract
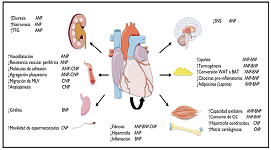
Circulating particles (extracellular vesicles) have the function of transmitting information between cells in biological processes such as vascular regulation, inflammation, coagulation, cell proliferation and apoptosis. It contains complex and diverse components, which are closely related to the occurrence and development of cardiovascular diseases. In the future, circulating particles (extracellular vesicles) can be used as clinical markers to reflect coagulation function, inflammatory reaction, tissue and organ damage, or as clinical treatment targets to regulate vascular homeostasis, correct coagulation, improve internal environment, and protect tissue and organ function, which has important research significance. In this paper, we summarize the relevant research progress of circulating particles (extracellular vesicles) in the field of cardiovascular surgery, and discuss the role of circulating particles (extracellular vesicles) in the process of related diseases, as well as its research and application prospects in the diagnosis and treatment of related diseases.
Keywords
References
- Russell AE, Sneider A, Witwer KW, et al. Biological membranes in EV biogenesis, stability, uptake, and cargo transfer: An ISEV position paper arising from the ISEV membranes and evs workshop. J Extracell Vesicles. 2019; 8(1): 1684862.
- Peterson DB, Sander T, Kaul S, et al. Comparative proteomic analysis of PAI-1 and TNF-alpha-derived endothelial microparticles. Proteomics. 2008; 8(12): 2430–2446.
- Kervadec A, Bellamy V, El Harane N, et al. Cardiovascular progenitor-derived extracellular vesicles recapitulate the beneficial effects of their parent cells in the treatment of chronic heart failure. J Heart Lung Transplant. 2016; 35(6): 795–807.
- Idriss NK, Blann AD, Sayed DM, et al. Circulating endothelial cells and platelet microparticles in mitral valve disease with and without atrialfibrillation. Angiology. 2015; 66(7): 631–637.
- Alegret JM, Martinez-Micaelo N, Aragones G, et al. Circulating endothelial microparticles are elevated in bicuspid aortic valve disease and related to aortic dilation. Int J Cardiol. 2016; 217: 35–41.
- Lin Z, Ci H, Li Y, et al. Endothelial microparticles are increased in congenital heart diseases and contribute to endothelial dysfunction. J Transl Med. 2017; 15(1): 4.
- Ou Z, Chang F, Luo D, et al. Endothelium-derived microparticles inhibit angiogenesis in the heart and enhance the inhibitory effects of hypercholesterolemia on angiogenesis. Am J Physiol Endocrinol Metab. 2011; 300(4): E661–E668.
- Habersberger J, Strang F, Scheichl A, et al. Circulating microparticles generate and transport monomeric C-reactive protein in patients with myocardial infarction. Cardiovascular Research. 2012; 96(1): 64–72.
- Arderiu G, Peña E, Badimon L. Angiogenic microvascular endothelial cells release microparticles rich in tissue factor that promotes postischemic collateral vessel formation. Arterioscl Throm Vasc Biol. 2015; 35(2): 348–357.
- Fontaine D, Pradier O, Hacquebard M, et al. Oxidative stress produced by circulating microparticles in on-pump but not in off-pump coronary surgery. Acta Cardiol. 2009; 64(6): 715–722.
- Gönença A, Hacişevki A, Bakkaloğlu B, et al. Oxidative stress is decreased in off-pump versus on-pump coronary artery surgery. J Biochem Mol Biol. 2006; 39(4): 377–382.
- Fu L, Hu X, Lin Z, et al. Circulating microparticles from patients with valvular heart disease and cardiac surgery inhibit endothelium-dependent vasodilation. Jthorac Cardiovasc Surg. 2015; 150(3): 666–672.
- Biróe E, Van Den Goor JM, De Mol BA, et al. Complement activation on the surface of cellderived microparticles during cardiac surgery with cardiopulmonary bypass is retransfusion of pericardial blood harmful? Perfusion. 2011; 26(1): 21–29.
- Krajewski S, Kurz J, Geisler T, et al. Combined blockade of ADP receptors and PI3-kinase p110 β fully prevents platelet and leukocyte activation during hypothermic extracorporeal circulation. Plos One. 2012; 7(6): E38455.
- Muriithi EW, Belcher PR, Day SP, et al. Heparin-induced platelet dysfunction and cardiopulmonary bypass. Ann Thorac Surg. 2000; 69(6): 1827-1832.
- Straub A, Breuer M, Wendel H P, et al. Critical temperature ranges of hypothermia-induced platelet activation: Possible implications for cooling patients in cardiac surgery. Thromb Haemost. 2007; 97(4): 608–616.
- Atherton J, Hampshire T, Englyst N, et al. The effect of circulating fresh blood through a micro-bypass circuit on platelet microparticles. Anaesthesia. 2012; 67(5): 555.
- Bosman GJ, Lasonder E, Groenen-dopp YA et al. The proteome of erythrocyte-derived microparticles from plasma: New clues for erythrocyte aging and vesiculation. J Proteomics. 2012; 76: 203–210.
- JY W, Gómez-marín O, Salerno TA, et al. Presurgical levels of circulating cell-derived microparticles discriminate between patients with and without transfusion in coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2015; 149(1): 305–311.
- Miyamoto S, Marcinkiewicz C, Edmunds LH r, et al. Measurement of platelet microparticles during cardiopulmonary bypass by means of captured ELISA for gpiib/iiia. Thromb Haemost. 1998; 80(2): 225–230.
- Nieuwland R, Berckmans RJ, Rotteveel-eijkman RC, et al. Cell-derived microparticles generated in patients during cardiopulmonary bypass are highly procoagulant. Circulation. 1997; 96(10): 3534–3541.
- Gemmell CH, Ramirez SM, Yeo EL, et al. Platelet activation in whole blood by artificial surfaces: Identification of platelet-derived microparticles and activated platelet binding to leukocytes as material-induced activation events. J Lab Clin Med. 1995; 125(2): 276–287.
- Jian YP, Yuan HX, Hu KH, et al. Protein compositions changes of circulating microparticles in patients with valvular heart disease subjected to cardiac surgery contribute to systemic inflammatory response and disorder of coagulation. Shock. 2019; 52(5): 487–496.
- Chung A, Wildhirt SM, Wang S, et al. Combined administration of nitric oxide gas and iloprost during cardiopulmonary bypass reduces platelet dysfunction: A pilot clinical study. J Thorac Cardiovasc Surg. 2005; 129(4): 782–790.
- Horn P, Cortese-krott MM, Amabile N, et al. Circulating microparticles carry a functional endothelial nitric oxide synthase that is decreased in patients with endothelial dysfunction. J Am Heart Assoc. 2012; 2(1): E003764.
- Klinkner DB, Densmore JC, Kaul S, et al. Endothelium-derived microparticles inhibit human cardiac valve endothelial cell function. Shock. 2006; 25(6): 575–580.
- Lovren F, Verma S. Evolving role of microparticles in the pathophysiology of endothelial dysfunction. Clin Chem. 2013; 59(8): 1166–1174.
- Jia L, Zhang W, Li T, et al. ERstress dependent microparticles derived from smooth muscle cells promote endothelial dysfunction during thoracic aortic aneurysm and dissection. Clin Sci (Lond). 2017; 131(12): 1287–1299.
- Diehl P, Nagy F, Sossong V, et al. Increased levels of circulating microparticles in patients with severe aortic valve stenosis. Thromb Haemost. 2008; 99(4): 711–719.
- Horn P, Erkilet G, Veulemans V, et al. Microparticle-induced coagulation relates to coronary artery atherosclerosis in severe aortic valve stenosis. Plos One. 2016; 11(3): E0151499.
- Gössl M, Khosla S, Zhang X, et al. Role of circulating osteogenic progenitor cells in calcific aortic stenosis. J Am Coll Cardiol. 2012; 60(19): 1945–1953.
- Kochtebane N, Passefort S, Choqueux C, et al. Release of leukotriene B4, transforming growth factor-beta1 and microparticles in relation to aortic valve calcification. J Heart Valve Dis. 2013; 22(6): 782–788.
- Dong Q, Chen Y, Liu W, et al. 25-Hydroxycholesterol promotes vascular calcification via activation of endoplasmic reticulum stress. Eur J Pharmacol. 2020; 880: 173165.
- Jung C, Lichtenauer M, Figulla HR, et al. Microparticles in patients undergoing transcatheter aortic valve implantation (TAVI). Heart Vessels. 2017; 32(4): 458-466.
- Sionis A, Suades R, Sans-rosello J, et al. Circulating microparticles are associated with clinical severity of persistent ST-segment elevation myocardial infarction complicated with cardiogenic shock. Int J Cardiol. 2018; 58: 249–256.
- Liu Y, He Z, Zhang Y, et al. Dissimilarity of increased phosphatidylserine-positive microparticles and associated coagulation activation in acute coronary syndromes. Coron Artery Dis. 2016; 27(5): 365–375.
- Georgescu A, Alexandru N, Andrei E, et al. Effects of transplanted circulating endothelial progenitor cells and platelet microparticles in atherosclerosis development. Biol Cell. 2016; 108(8): 219–243.
- Barile L, Lionetti V, Cervio E, et al. Extracellular vesicles from human cardiac progenitor cells inhibit cardiomyocyte apoptosis and improve cardiac function after myocardial infarction. Cardiovasc Res. 2014; 103(4): 530–541.
- Chen Y, Yuan H, Ou Z, et al. Microparticles (exosomes)and atherosclerosis. Curr Atheroscler Rep. 2020; 22(6): 23.
- Camera M, Brambilla M, Canzano P, et al. Association of microvesicles with graft patency in patients undergoing CABG surgery. J Am Coll Cardiol. 2020; 75(22): 2819–2832.
- Chatterjee D, Moore C, Gao B, et al. Prevalence of polyreactive innate clones among graft-infiltrating B cells in human cardiac allograft vasculopathy. J Heart Lung Transplant. 2018; 37(3): 385–393.
- Wu C, Zhao Y, Xiao X, et al. Graft-infiltrating macrophages adopt an M2 phenotype and are inhibited by purinergic receptor P2X7 antagonist in chronic rejection. Am J Transplant. 2016; 16(9): 2563–2573.
- Lin CM, Plenter RJ, Coulombe M, et al. Interferon gamma and contact-dependent cytotoxicity are each rate limiting for natural killer cell-mediatedantibody-dependent chronic rejection. Am J Transplant. 2016; 16(11): 3121–3130.
- Edwards LA, Nowocin AK, Jafari NV, et al. Chronic rejection of cardiac allografts is associated with increased lymphatic flow and cellular trafficking. Circulation. 2018; 137(5): 488–503.
- Huibers MM, Gareau AJ, Beerthuijzen JM, et al. Donor-specific antibodies are produced locally in ectopic lymphoid structures in cardiac allografts. Am J Transplant. 2017; 17(1): 246–254.
- Singh N, Van Craeyveld E, Tjwa M, et al. Circulating apoptotic endothelial cells and apoptotic endothelial microparticles independently predict the presence of cardiac allograft vasculopathy. J Am Coll Cardiol. 2012; 60(4): 324–331.
- Garcia S, Chirinos J, Jimenez J, et al. Phenotypic assessment of endothelial microparticles in patients with heart failure and after heart transplantation: Switch from cell activation to apoptosis. J Heart Lung Transplant. 2005; 24(12): 2184–2189.
- Singh N, Vanhaecke J, Van Cleemput J, et al. Markers of endothelial injury and platelet microparticles are distinct in patients with stable native coronary artery disease and with cardiac allograft vasculopathy. Int J Cardiol. 2015; 179(2015): 331-333.
- Densmore JC, Signorino PR, Ou J, et al. Endothelium-derived microparticles induce endothelial dysfunction and acute lung injury. Shock. 2006; 26(5): 464–471.
- Lanyu Z, Feilong H. Emerging role of extracellular vesicles in lung injury and inflammation. Biomed Pharmacother. 2019; 113: 108748.
- Yuan H, Chen C Li Y, et al. Circulating extracellular vesicles from patients with valvular heart disease induce neutrophil chemotaxis via FOXO3a and the inhibiting role of dexmedetomidine. Am J Physiol Endocrinol Metab. 2020; 319(1): E217–E231.
- Sullo N, Mariani S, Jntala M, et al. An observational cohort feasibility study to identify microvesicle and micro-RNA biomarkers of acute kidney injury following pediatric cardiac surgery. Pediatr Crit Care Me. 2018; 19(9): 816–830.
- Schiro A, Wilkinson FL, Weston R, et al. Elevated levels of endothelial-derived microparticles, and serum CXCL9 and SCGF-beta are associated with unstable asymptomatic carotid plaques. Sci Rep. 2015; 5(1): 16658.
- Sarlon-bartoli G, Bennis Y, Lacroix R, et al. Plasmatic level of leukocyte-derived microparticles is associated with unstable plaque in asymptomatic patients with high-grade carotid stenosis. J Am Coll Cardiol. 2013; 62(16): 1436–1441.
- Ivak P, Pitha J, Wohlfahrt P, et al. Biphasic response in number of stem cells and endothelial progenitor cells after left ventricular assist device implantation: A 6 month follow-up. Int J Cardiol. 2016; 218: 98–103.
- Sansone R, Stanske B, Keymel S, et al. Macrovascular and microvascular function after implantation of left ventricular assist devices in endstage heart failure: Role of microparticles. J Heart Lung Transplant. 2015; 34(7): 921–932.
- Nascimbene A, Hernandez R, George JK, et al. Association between cell-derived microparticles and adverse events in patients with nonpulsatile left ventricular assist devices. J Heart Lung Transplant. 2014; 33(5): 470–477.
- Sander TL, Ou JS, Densmore JC, et al. Protein composition of plasminogen activator inhibitor type 1-derived endothelial microparticles. Shock. 2008; 29(4): 504–511.
- Braga-lagache S, Buchs N, Iacovache MI, et al. Robust label-free, quantitative profiling of circulating plasma microparticle (MP)associated proteins. Mol Cell Proteomics. 2016; 15(12): 3640–3652.
- Baysa A, Fedorov A, Kondratov K, et al. Release of mitochondrial and nuclear DNA during on-pump heart surgery: Kinetics and relation to extracellular vesicles. J Cardiovasc Transl Res. 2019; 12(3): 184-192.
- Zhan R, Xu K, Pan J, et al. Long noncoding RNA MEG3 mediated angiogenesis after cerebral infarction through regulating p53/NOX4 axis. Biochem Biophys Res Commun. 2017; 490(3): 700–706.
- Zhuo X, Wu Y, Yang Y, et al. Lncrna AK094457 promotes angii-mediated hypertension and endothelial dysfunction through suppressing of activation of ppargamma. Life Sci. 2019; 233: 116745.
- Yan B, Yao J, Liu JY, et al. Lncrna-MIAT regulates microvascular dysfunction by functioning as a competingendogenous RNA. Circ Res. 2015; 116(7): 1143-1156.
- Zhang H, Xu Q, Thakur A, et al. Endothelial dysfunction in diabetes and hypertension: Role of micrornas and long non-coding rnas. Life Sci. 2018; 213: 258–268.
- Wu C, Wang Y, Jin B, et al. Senescence-associated long non-coding RNA (SALNR)delays oncogeneinduced senescence through NF90 regulation. J Biol Chem. 2015; 290(50): 30175–30192.
- Rognoni A, Cavallino C, Lupi A, et al. Novelbiomarkers in the diagnosis of acute coronary syndromes: The role of circulating mirnas. Expert Rev Cardiovasc Ther. 2014; 12(9): 1119–1124.
- Kumar S, Williams D, Sur S, et al. Role offlow-sensitive micrornas and long noncoding rnas in vascular dysfunction and atherosclerosis. Vascul Pharmacol. 2019; 114: 76–92.
- Vilahur G, Cubedo J, Padro T, et al. Roflumilast-induced local vascular injury is associated with a coordinated proteome and microparticle change in the systemic circulation in pigs. Toxicol Pathol. 2015; 43(4): 569–580.
- Desai PH, Kurian D, Thirumavalavan N, et al. A randomized clinical trial investigating the relationship between aprotinin and hypercoagulability in off-pump coronary surgery. Anesth Analg. 2009; 109(5): 1387–1394.
- Kuo H, Hsieh CC, Wang S, et al. Simvastatin attenuates cardiac fibrosis via regulation of cardiomyocyte-derived exosome secretion. J Clin Med. 2019; 8(6): 794.
- Cheng G, Shan X, Wang X, et al. Endothelial damage effects of circulating microparticles from patients with stable angina are reduced by aspirin through ERK/p38 mapks pathways. Cardiovasc Ther. 2017; 35(4): 12274.
- Ma J, Chen Y, Chen C, et al. The correlation between concentrations of size-dependent circulating microparticles from patients and the dose of positive inotropic medicine undergoing cardiac surgery with cardiopulmonary bypass (Chinese). Chinese Journal of Arteriosclerosis. 2020; 28(10): 847–851.
Supporting Agencies
Copyright (c) 2020 Kaifeng Liang, Jingsong Ou

This work is licensed under a Creative Commons Attribution 4.0 International License.

This site is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0).

Prof. Prakash Deedwania
University of California,
San Francisco, United States




