
Asia Pacific Academy of Science Pte. Ltd. (APACSCI) specializes in international journal publishing. APACSCI adopts the open access publishing model and provides an important communication bridge for academic groups whose interest fields include engineering, technology, medicine, computer, mathematics, agriculture and forestry, and environment.
Macrophages in the pathogenesis of psoriasis and anti-psoriatic nanotherapies
Vol 39, Issue 2, 2025
Download PDF
Abstract
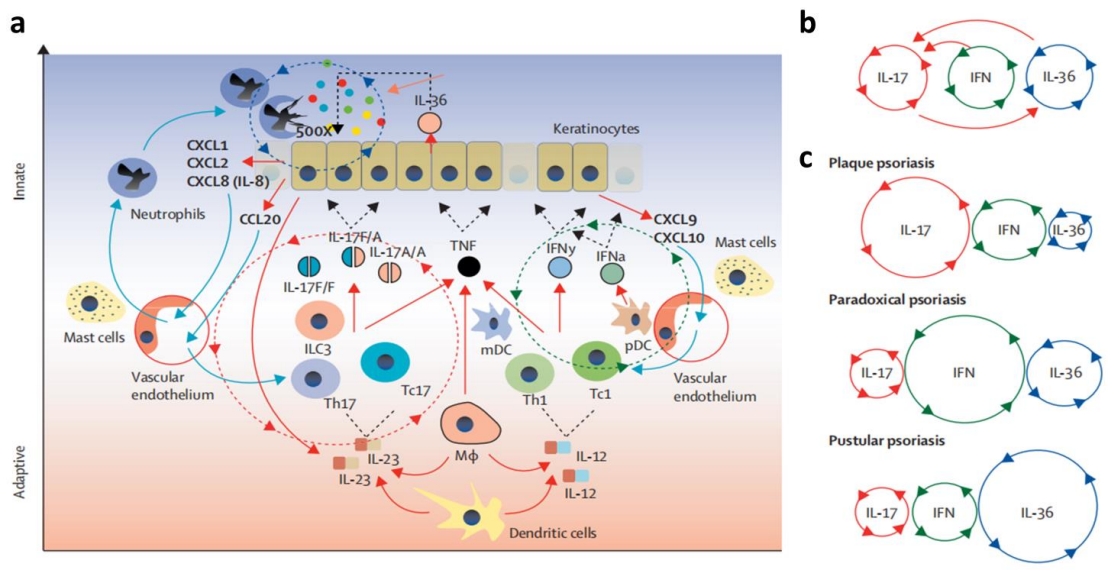
Psoriasis is a common, chronic, and inflammatory skin disease. Macrophages account for about 61.3% of the inflammatory cells infiltrating psoriatic lesions. Modulating macrophage polarization, inhibiting their infiltration, and targeting the secretion of inflammatory factors and associated inflammatory pathways by these cells can alleviate psoriasis symptoms and inflammation. Moreover, nanomaterials as novel drug carriers, offer unique advantages such as large surface area, easy modification, high biocompatibility, good biodegradability, enhanced systemic adsorption, etc. Nanomaterials have great potential for efficient drug delivery and release, as well as improving therapeutic efficacy while reducing adverse effects. By systematically addressing the role of macrophages in psoriasis pathogenesis and the potential of nanomaterials in treating psoriasis through modulating macrophages, this review enhances our understanding of the disease mechanism and holds promise for novel therapeutic breakthroughs and advancements in the future treatment of psoriasis.
Keywords
References
- Boehncke WH, Schön MP. Psoriasis. The Lancet. 2015; 386(9997): 983-994. doi: 10.1016/S0140-6736(14)61909-7
- Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. The Lancet. 2021; 397(10281): 1301-1315. doi: 10.1016/S0140-6736(20)32549-6
- Wang Y, Qi C, Feng F, et al. Resveratrol Ameliorates Imiquimod-Induced Psoriasis-Like Mouse Model via Reducing Macrophage Infiltration and Inhibiting Glycolysis. Journal of Inflammation Research. 2023; 16: 3823-3836. doi: 10.2147/jir.s416417
- Leite Dantas R, Masemann D, Schied T, et al. Macrophage‐mediated psoriasis can be suppressed by regulatory T lymphocytes. The Journal of Pathology. 2016; 240(3): 366-377. doi: 10.1002/path.4786
- Xia T, Fu S, Yang R, et al. Advances in the study of macrophage polarization in inflammatory immune skin diseases. Journal of Inflammation. 2023; 20(1). doi: 10.1186/s12950-023-00360-z
- Greb JE, Goldminz AM, Elder JT, et al. Psoriasis. Nature Reviews Disease Primers. 2016; 2(1). doi: 10.1038/nrdp.2016.82
- Sarma N. Evidence and Suggested Therapeutic Approach in Psoriasis of Difficult-to-treat Areas: Palmoplantar Psoriasis, Nail Psoriasis, Scalp Psoriasis, and Intertriginous Psoriasis. Indian Journal of Dermatology. 2017; 62(2): 113-122. doi: 10.4103/ijd.IJD_539_16
- Yona S, Gordon S. From the Reticuloendothelial to Mononuclear Phagocyte System – The Unaccounted Years. Frontiers in Immunology. 2015; 6. doi: 10.3389/fimmu.2015.00328
- Stuart LM, Ezekowitz RAB. Phagocytosis: elegant complexity. Immunity. 2005; 22(5): 539-550. doi: 10.1016/j.immuni.2005.05.002
- Martinez FO, Gordon S. The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Reports. 2014; 6. doi: 10.12703/p6-13
- Kim HJ, Jang J, Lee E, et al. Decreased expression of response gene to complement 32 in psoriasis and its association with reduced M2 macrophage polarization. The Journal of Dermatology. 2019; 46(2): 166-168. doi: 10.1111/1346-8138.14733
- Lin SH, Chuang HY, Ho JC, et al. Treatment with TNF-α inhibitor rectifies M1 macrophage polarization from blood CD14+ monocytes in patients with psoriasis independent of STAT1 and IRF-1 activation. Journal of Dermatological Science. 2018; 91(3): 276-284. doi: 10.1016/j.jdermsci.2018.05.009
- Sun Q, Hu S, Lou Z, et al. The macrophage polarization in inflammatory dermatosis and its potential drug candidates. Biomedicine & Pharmacotherapy. 2023; 161: 114469. doi: 10.1016/j.biopha.2023.114469
- Sans-Fons MG, Yeramian A, Pereira-Lopes S, et al. Arginine Transport Is Impaired in C57Bl/6 Mouse Macrophages as a Result of a Deletion in the Promoter of Slc7a2 (CAT2), and Susceptibility to Leishmania Infection Is Reduced. The Journal of Infectious Diseases. 2013; 207(11): 1684-1693. doi: 10.1093/infdis/jit084
- Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. Journal of Clinical Investigation. 2012; 122(3): 787-795. doi: 10.1172/jci59643
- Schenk M, Bouchon A, Seibold F, et al. TREM-1–expressing intestinal macrophages crucially amplify chronic inflammation in experimental colitis and inflammatory bowel diseases. Journal of Clinical Investigation. 2007; 117(10): 3097-3106. doi: 10.1172/jci30602
- Mosser DM, Edwards JP. Erratum: Exploring the full spectrum of macrophage activation. Nature Reviews Immunology. 2010; 10(6): 460-460. doi: 10.1038/nri2788
- Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nature Reviews Immunology. 2011; 11(11): 723-737. doi: 10.1038/nri3073
- Geissmann F, Jung S, Littman DR. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity. 2003; 19(1): 71-82. doi: 10.1016/S1074-7613(03)00174-2
- Hanna RN, Carlin LM, Hubbeling HG, et al. The transcription factor NR4A1 (Nur77) controls bone marrow differentiation and the survival of Ly6C− monocytes. Nature Immunology. 2011; 12(8): 778-785. doi: 10.1038/ni.2063
- Ge H, Mao Y, Chen W, et al. Stress aggravates imiquimod-induced psoriasiform inflammation by promoting M1 macrophage polarization. International Immunopharmacology. 2023; 124: 110899. doi: 10.1016/j.intimp.2023.110899
- Lu CH, Lai CY, Yeh DW, et al. Involvement of M1 Macrophage Polarization in Endosomal Toll-Like Receptors Activated Psoriatic Inflammation. Mediators of Inflammation. 2018; 2018: 1-14. doi: 10.1155/2018/3523642
- Lu Y, Zhu W, Zhang GX, et al. Adenosine A2A receptor activation regulates the M1 macrophages activation to initiate innate and adaptive immunity in psoriasis. Clinical Immunology. 2024; 266: 110309. doi: 10.1016/j.clim.2024.110309
- Oh-Oka K, Sugaya M, Takahashi N, et al. CD96 Blockade Ameliorates Imiquimod-Induced Psoriasis-like Dermatitis via Suppression of IL-17A Production by Dermal γδ T Cells. The Journal of Immunology. 2022. doi: 10.4049/jimmunol.1601607
- Liu Y, Qin G, Meng Z, et al. IL-1β, IL-17A and combined phototherapy predicts higher while previous systemic biologic treatment predicts lower treatment response to etanercept in psoriasis patients. Inflammopharmacology. 2018; 27(1): 57-66. doi: 10.1007/s10787-018-0530-9
- Ciesla M, Kolarz B, Majdan M, et al. POS0191 the value of mir-20B, MIR-22, MIR-26A, MIR-125B AND MIR-221 in rheumatoid arthritis. Annals of the Rheumatic Diseases. 2021; 80: 309-310. doi: 10.1136/annrheumdis-2021-eular.443
- Yang X, Zhao Q, Wang X, et al. Investigation of Clostridium butyricum on atopic dermatitis based on gut microbiota and TLR4/MyD88/ NF-κB signaling pathway. Technology and Health Care; 2025.
- Grine L, Dejager L, Libert C, et al. An inflammatory triangle in psoriasis: TNF, type I IFNs and IL-17. Cytokine & Growth Factor Reviews. 2015; 26(1): 25-33. doi: 10.1016/j.cytogfr.2014.10.009
- Brembilla NC, Senra L, Boehncke WH. The IL-17 Family of Cytokines in Psoriasis: IL-17A and Beyond. Frontiers in Immunology. 2018; 9. doi: 10.3389/fimmu.2018.01682
- von Stebut E, Boehncke WH, Ghoreschi K, et al. IL-17A in Psoriasis and Beyond: Cardiovascular and Metabolic Implications. Frontiers in Immunology. 2020; 10. doi: 10.3389/fimmu.2019.03096
- Fischer-Riepe L, Daber N, Schulte-Schrepping J, et al. CD163 expression defines specific, IRF8-dependent, immune-modulatory macrophages in the bone marrow. Journal of Allergy and Clinical Immunology. 2020.
- Mahil SK, Capon F, Barker JN. Update on psoriasis immunopathogenesis and targeted immunotherapy. Seminars in Immunopathology. 2015; 38(1): 11-27. doi: 10.1007/s00281-015-0539-8
- Zaba LC, Cardinale I, Gilleaudeau P, et al. Amelioration of epidermal hyperplasia by TNF inhibition is associated with reduced Th17 responses. The Journal of Experimental Medicine. 2007; 204(13): 3183-3194. doi: 10.1084/jem.20071094
- Ward NL, Loyd CM, Wolfram JA, et al. Depletion of antigen-presenting cells by clodronate liposomes reverses the psoriatic skin phenotype in KC-Tie2 mice. British Journal of Dermatology. 2011; 164(4): 750-758. doi: 10.1111/j.1365-2133.2010.10129.x
- Nguyen CTH, Kambe N, Yamazaki F, et al. Up-regulated expression of CD86 on circulating intermediate monocytes correlated with disease severity in psoriasis. Journal of Dermatological Science. 2018; 90(2): 135-143. doi: 10.1016/j.jdermsci.2018.01.005
- Golden JB, Groft SG, Squeri MV, et al. Chronic Psoriatic Skin Inflammation Leads to Increased Monocyte Adhesion and Aggregation. The Journal of Immunology. 2015; 195(5): 2006-2018. doi: 10.4049/jimmunol.1402307
- Wang H, Peters T, Sindrilaru A, et al. Key Role of Macrophages in the Pathogenesis of CD18 Hypomorphic Murine Model of Psoriasis. Journal of Investigative Dermatology. 2009; 129(5): 1100-1114. doi: 10.1038/jid.2009.43
- Sa SM, Valdez PA, Wu J, et al. The effects of IL-20 subfamily cytokines on reconstituted human epidermis suggest potential roles in cutaneous innate defense and pathogenic adaptive immunity in psoriasis. The Journal of Immunology. 2007; 178(11): 7487-7487. doi: 10.4049/jimmunol.178.11.7487-a
- Fonseca-Camarillo G, Furuzawa-Carballeda J, Llorente L, et al. IL-10— and IL-20—Expressing Epithelial and Inflammatory Cells are Increased in Patients with Ulcerative Colitis. Journal of Clinical Immunology. 2012; 33(3): 640-648. doi: 10.1007/s10875-012-9843-4
- Wang L, Yang L, Gao L, et al. A functional promoter polymorphism in monocyte chemoattractant protein‐1 is associated with psoriasis. International Journal of Immunogenetics. 2007; 35(1): 45-49. doi: 10.1111/j.1744-313x.2007.00734.x
- Wang H. Activated macrophages are essential in a murine model for T cell-mediated chronic psoriasiform skin inflammation. Journal of Clinical Investigation. 2006; 116(8): 2105-2114. doi: 10.1172/jci27180
- Zhu Y, Wu Z, Yan W, et al. Allosteric inhibition of SHP2 uncovers aberrant TLR7 trafficking in aggravating psoriasis. EMBO Molecular Medicine. 2021; 14(3). doi: 10.15252/emmm.202114455
- Kim J, Krueger JG. The Immunopathogenesis of Psoriasis. Dermatologic Clinics. 2015; 33(1): 13-23. doi: 10.1016/j.det.2014.09.002
- Kuraitis D, Rosenthal N, Boh E, et al. Macrophages in dermatology: pathogenic roles and targeted therapeutics. Archives of Dermatological Research. 2021; 314(2): 133-140. doi: 10.1007/s00403-021-02207-0
- Paulnock DM. Macrophage activation by T cells. Current Opinion in Immunology. 1992; 4(3): 344-349. doi: 10.1016/0952-7915(92)90087-U
- Fuentes-Duculan J, Suárez-Fariñas M, Zaba LC, et al. A Subpopulation of CD163-Positive macrophages is classically activated in psoriasis. Journal of Investigative Dermatology. 2010; 130(10): 2412-2422. doi: 10.1038/jid.2010.165
- Malissen B, Tamoutounour S, Henri S. The origins and functions of dendritic cells and macrophages in the skin. Nature Reviews Immunology. 2014; 14(6): 417-428. doi: 10.1038/nri3683
- Lim H, Yo S, Lee M, et al. Potential inhibitory effects of the traditional herbal prescription Hyangso-san against skin inflammation via inhibition of chemokine production and inactivation of STAT1 in HaCaT keratinocytes. Molecular Medicine Reports. 2017; 17(2): 2515-2522. doi: 10.3892/mmr.2017.8172
- Park CH, Min SY, Yu HW, et al. Effects of Apigenin on RBL-2H3, RAW264.7, and HaCaT Cells: Anti-Allergic, Anti-Inflammatory, and Skin-Protective Activities. International Journal of Molecular Sciences. 2020; 21(13): 4620. doi: 10.3390/ijms21134620
- Li R, Xiong Y, Ma L, et al. Neutrophil extracellular traps promote macrophage inflammation in psoriasis. Clinical Immunology. 2024; 266: 110308. doi: 10.1016/j.clim.2024.110308
- Hetru C, Hoffmann JA. NF- B in the Immune Response of Drosophila. Cold Spring Harbor Perspectives in Biology. 2009; 1(6): a000232-a000232. doi: 10.1101/cshperspect.a000232
- Liu T, Zhang L, Joo D, et al. NF-κB signaling in inflammation. Signal Transduction and Targeted Therapy. 2017; 2(1). doi: 10.1038/sigtrans.2017.23
- Cildir G, Low KC, Tergaonkar V. Noncanonical NF-κB Signaling in Health and Disease. Trends in Molecular Medicine. 2016; 22(5): 414-429. doi: 10.1016/j.molmed.2016.03.002
- Alcamo E, Hacohen N, Schulte LC, et al. Requirement for the NF-κB Family Member RelA in the Development of Secondary Lymphoid Organs. The Journal of Experimental Medicine. 2002; 195(2): 233-244. doi: 10.1084/jem.20011885
- Hayden MS, Ghosh S. Shared Principles in NF-κB Signaling. Cell. 2008; 132(3): 344-362. doi: 10.1016/j.cell.2008.01.020
- Schröfelbauer B, Polley S, Behar M, et al. NEMO Ensures Signaling Specificity of the Pleiotropic IKKβ by Directing Its Kinase Activity toward IκBα. Molecular Cell. 2012; 47(1): 111-121. doi: 10.1016/j.molcel.2012.04.020
- Oeckinghaus A, Ghosh S. The NF- B Family of Transcription Factors and Its Regulation. Cold Spring Harbor Perspectives in Biology. 2009; 1(4): a000034-a000034. doi: 10.1101/cshperspect.a000034
- Gao S, Mao F, Zhang B, et al. Mouse bone marrow-derived mesenchymal stem cells induce macrophage M2 polarization through the nuclear factor-κB and signal transducer and activator of transcription 3 pathways. Experimental Biology and Medicine. 2014; 239(3): 366-375. doi: 10.1177/1535370213518169
- Takuathung MN, Potikanond S, Sookkhee S, et al. Anti-psoriatic and anti-inflammatory effects of Kaempferia parviflora in keratinocytes and macrophage cells. Biomedicine & Pharmacotherapy. 2021; 143: 112229. doi: 10.1016/j.biopha.2021.112229
- Chen XX, Tang L, Fu YM, et al. Paralemmin-3 contributes to lipopolysaccharide-induced inflammatory response and is involved in lipopolysaccharide-Toll-like receptor-4 signaling in alveolar macrophages. International Journal of Molecular Medicine. 2017; 40(6): 1921-1931. doi: 10.3892/ijmm.2017.3161
- Sae-Wong C, Matsuda H, Tewtrakul S, et al. Suppressive effects of methoxyflavonoids isolated from Kaempferia parviflora on inducible nitric oxide synthase (iNOS) expression in RAW 264.7 cells. Journal of Ethnopharmacology. 2011; 136(3): 488-495. doi: 10.1016/j.jep.2011.01.013
- Tewtrakul S, Subhadhirasakul S. Effects of compounds from Kaempferia parviflora on nitric oxide, prostaglandin E2 and tumor necrosis factor-alpha productions in RAW264.7 macrophage cells. Journal of Ethnopharmacology. 2008; 120(1): 81-84. doi: 10.1016/j.jep.2008.07.033
- Thatikonda S, Pooladanda V, Sigalapalli DK, et al. Piperlongumine regulates epigenetic modulation and alleviates psoriasis-like skin inflammation via inhibition of hyperproliferation and inflammation. Cell Death & Disease. 2020; 11(1). doi: 10.1038/s41419-019-2212-y
- Wang W, Qu R, Wang X, et al. GDF11 Antagonizes Psoriasis-like Skin Inflammation via Suppression of NF-κB Signaling Pathway. Inflammation. 2018; 42(1): 319-330. doi: 10.1007/s10753-018-0895-3
- Shangguan Y, Chen Y, Ma Y, et al. Salubrinal protects against inflammatory response in macrophage and attenuates psoriasiform skin inflammation by antagonizing NF-κB signaling pathway. Biochemical and Biophysical Research Communications. 2022; 589: 63-70. doi: 10.1016/j.bbrc.2021.11.066
- Catharino A, Daiha E, Carvalho C, et al. Possible correlations between annular pustular psoriasis and Noonan syndrome. Journal of the European Academy of Dermatology and Venereology. 2015; 30(12). doi: 10.1111/jdv.13521
- Meng Q, Bai M, Guo M, et al. Inhibition of Serum- and Glucocorticoid-Regulated Protein Kinase-1 Aggravates Imiquimod-Induced Psoriatic Dermatitis and Enhances Proinflammatory Cytokine Expression through the NF-kB Pathway. Journal of Investigative Dermatology. 2023; 143(6): 954-964. doi: 10.1016/j.jid.2022.12.013
- Welters ID, Fimiani C, Bilfinger TV, et al. NF- κ B, nitric oxide and opiate signaling. Medical Hypotheses. 2000; 54(2): 263-268. doi: 10.1054/mehy.1999.0032
- Xu N, Yuan H, Liu W, et al. Activation of RAW264.7 mouse macrophage cells in vitro through treatment with recombinant ricin toxin-binding subunit B: Involvement of protein tyrosine, NF-κB and JAK-STAT kinase signaling pathways. International Journal of Molecular Medicine. 2013; 32(3): 729-735. doi: 10.3892/ijmm.2013.1426
- Funes SC, Rios M, Escobar‐Vera J, et al. Implications of macrophage polarization in autoimmunity. Immunology. 2018; 154(2): 186-195. doi: 10.1111/imm.12910
- Liu Y, Liu Z, Tang H, et al. The N6-methyladenosine (m6A)-forming enzyme METTL3 facilitates M1 macrophage polarization through the methylation of STAT1 mRNA. American Journal of Physiology-Cell Physiology. 2019; 317(4): C762-C775. doi: 10.1152/ajpcell.00212.2019
- Ren J, Han X, Lohner H, et al. Serum- and Glucocorticoid-Inducible Kinase 1 Promotes Alternative Macrophage Polarization and Restrains Inflammation through FoxO1 and STAT3 Signaling. The Journal of Immunology. 2021; 207(1): 268-280. doi: 10.4049/jimmunol.2001455
- Li L, Zhang H yu, Zhong X qin, et al. PSORI-CM02 formula alleviates imiquimod-induced psoriasis via affecting macrophage infiltration and polarization. Life Sciences. 2020; 243: 117231. doi: 10.1016/j.lfs.2019.117231
- Ma Y, Kim BH, Yun SK, et al. Centipeda minima Extract Inhibits Inflammation and Cell Proliferation by Regulating JAK/STAT Signaling in Macrophages and Keratinocytes. Molecules. 2023; 28(4): 1723. doi: 10.3390/molecules28041723
- Li X, Jiang M, Chen X, et al. Etanercept alleviates psoriasis by reducing the Th17/Treg ratio and promoting M2 polarization of macrophages. Immunity, Inflammation and Disease. 2022; 10(12). doi: 10.1002/iid3.734
- Hou Y, Zhu L, Tian H, et al. IL-23-induced macrophage polarization and its pathological roles in mice with imiquimod-induced psoriasis. Protein & Cell. 2018; 9(12): 1027-1038. doi: 10.1007/s13238-018-0505-z
- Reich K, Papp KA, Blauvelt A, et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials. The Lancet. 2017; 390(10091): 276-288. doi: 10.1016/S0140-6736(17)31279-5
- Jiang BH, Liu LZ. PI3K/PTEN Signaling in Angiogenesis and Tumorigenesis. Advances in Cancer Research. 2009; 102: 19-65. doi: 10.1016/S0065-230X(09)02002-8
- He Y, Sun MM, Zhang GG, et al. Targeting PI3K/Akt signal transduction for cancer therapy. Signal Transduction and Targeted Therapy. 2021; 6(1). doi: 10.1038/s41392-021-00828-5
- Murthy SS, Tosolini A, Taguchi T, et al. Mapping of AKT3, encoding a member of the Akt/protein kinase B family, to human and rodent chromosomes by fluorescence in situ hybridization. Cytogenetic and Genome Research. 2000; 88(1-2): 38-40. doi: 10.1159/000015481
- Xue C, Li G, Lu J, et al. Crosstalk between circRNAs and the PI3K/AKT signaling pathway in cancer progression. Signal Transduction and Targeted Therapy. 2021; 6(1). doi: 10.1038/s41392-021-00788-w
- Song G, Ouyang G, Bao S. The activation of Akt/PKB signaling pathway and cell survival. Journal of Cellular and Molecular Medicine. 2005; 9(1): 59-71. doi: 10.1111/j.1582-4934.2005.tb00337.x
- Luyendyk JP, Schabbauer GA, Tencati M, et al. Genetic Analysis of the Role of the PI3K-Akt Pathway in Lipopolysaccharide-Induced Cytokine and Tissue Factor Gene Expression in Monocytes/Macrophages. The Journal of Immunology. 2008; 180(6): 4218-4226. doi: 10.4049/jimmunol.180.6.4218
- Weichhart T, Säemann MD. The multiple facets of mTOR in immunity. Trends in Immunology. 2009; 30(5): 218-226. doi: 10.1016/j.it.2009.02.002
- Arranz A, Doxaki C, Vergadi E, et al. Akt1 and Akt2 protein kinases differentially contribute to macrophage polarization. Proceedings of the National Academy of Sciences. 2012; 109(24): 9517-9522. doi: 10.1073/pnas.1119038109
- Vergadi E, Ieronymaki E, Lyroni K, et al. Akt Signaling Pathway in Macrophage Activation and M1/M2 Polarization. The Journal of Immunology. 2017; 198(3): 1006-1014. doi: 10.4049/jimmunol.1601515
- Gu S, Dai H, Zhao X, et al. AKT3 deficiency in M2 macrophages impairs cutaneous wound healing by disrupting tissue remodeling. Aging. 2020; 12(8): 6928-6946. doi: 10.18632/aging.103051
- Chamcheu JC, Pal HC, Siddiqui IA, et al. Prodifferentiation, Anti-Inflammatory and Antiproliferative Effects of Delphinidin, a Dietary Anthocyanidin, in a Full-Thickness Three-Dimensional Reconstituted Human Skin Model of Psoriasis. Skin Pharmacology and Physiology. 2015; 28(4): 177-188. doi: 10.1159/000368445
- Buerger C, Malisiewicz B, Eiser A, et al. Mammalian target of rapamycin and its downstream signalling components are activated in psoriatic skin. British Journal of Dermatology. 2013; 169(1): 156-159. doi: 10.1111/bjd.12271
- Rosenberger C, Solovan C, Rosenberger AD, et al. Upregulation of Hypoxia-Inducible Factors in Normal and Psoriatic Skin. Journal of Investigative Dermatology. 2007; 127(10): 2445-2452. doi: 10.1038/sj.jid.5700874
- Huang T, Lin X, Meng X, et al. Phosphoinositide-3 Kinase/Protein Kinase-B/Mammalian Target of Rapamycin Pathway in Psoriasis Pathogenesis. A Potential Therapeutic Target? Acta Dermato Venereologica. 2014; 94(4): 371-379. doi: 10.2340/00015555-1737
- Jiang Z, Zhang Y, Zhang Y, et al. Cancer Derived Exosomes Induce Macrophages Immunosuppressive Polarization to Promote Bladder Cancer Progression. Cell Commun Signal. 2021; 19: 93. doi: 10.1186/s12964-021-00768-1
- Jeon H, Oh S, Kum E, et al. Immunomodulatory Effects of an Aqueous Extract of Black Radish on Mouse Macrophages via the TLR2/4-Mediated Signaling Pathway. Pharmaceuticals. 2022; 15(11): 1376. doi: 10.3390/ph15111376
- Du M, Chen ZJ. DNA-induced liquid phase condensation of cGAS activates innate immune signaling. Science. 2018; 361(6403): 704-709. doi: 10.1126/science.aat1022
- Andreeva L, Hiller B, Kostrewa D, et al. cGAS senses long and HMGB/TFAM-bound U-turn DNA by forming protein–DNA ladders. Nature. 2017; 549(7672): 394-398. doi: 10.1038/nature23890
- Decout A, Katz JD, Venkatraman S, et al. The cGAS–STING pathway as a therapeutic target in inflammatory diseases. Nature Reviews Immunology. 2021; 21(9): 548-569. doi: 10.1038/s41577-021-00524-z
- Pan J, Fei C, Hu Y, et al. Current understanding of the cGAS-STING signaling pathway: Structure, regulatory mechanisms, and related diseases. Zoological Research. 2023; 44(1): 183-218. doi: 10.24272/j.issn.2095-8137.2022.464
- Samson N, Ablasser A. The cGAS–STING pathway and cancer. Nature Cancer. 2022; 3(12): 1452-1463. doi: 10.1038/s43018-022-00468-w
- Chen C, Xu P. Cellular functions of cGAS-STING signaling. Trends in Cell Biology. 2023; 33(8): 630-648. doi: 10.1016/j.tcb.2022.11.001
- Hopfner KP, Hornung V. Molecular mechanisms and cellular functions of cGAS–STING signalling. Nature Reviews Molecular Cell Biology. 2020; 21(9): 501-521. doi: 10.1038/s41580-020-0244-x
- Pan Y, You Y, Sun L, et al. The STING antagonist H‐151 ameliorates psoriasis via suppression of STING/NF‐κB‐mediated inflammation. British Journal of Pharmacology. 2021; 178(24): 4907-4922. doi: 10.1111/bph.15673
- Zhang Z, Zhou D, Li Z, et al. A Nanoinhibitor Targeting cGAS‐STING Pathway to Reverse the Homeostatic Imbalance of Inflammation in Psoriasis. Angewandte Chemie. 2023; 136(2). doi: 10.1002/ange.202316007
- Johansen C, Kragballe K, Westergaard M, et al. The mitogen-activated protein kinases p38 and ERK1/2 are increased in lesional psoriatic skin. British Journal of Dermatology. 2005; 152(1): 37-42. doi: 10.1111/j.1365-2133.2004.06304.x
- Takahashi H, Ibe M, Nakamura S, et al. Extracellular regulated kinase and c-Jun N-terminal kinase are activated in psoriatic involved epidermis. Journal of Dermatological Science. 2002; 30(2): 94-99. doi: 10.1016/S0923-1811(02)00064-6
- Funding AT, Johansen C, Kragballe K, et al. Mitogen- and Stress-Activated Protein Kinase 2 and Cyclic AMP Response Element Binding Protein are Activated in Lesional Psoriatic Epidermis. Journal of Investigative Dermatology. 2007; 127(8): 2012-2019. doi: 10.1038/sj.jid.5700821
- Mavropoulos A, Rigopoulou EI, Liaskos C, et al. The Role of p38 MAPK in the Aetiopathogenesis of Psoriasis and Psoriatic Arthritis. Clinical and Developmental Immunology. 2013; 2013: 1-8. doi: 10.1155/2013/569751
- Fu J, Zeng Z, Zhang L, et al. 4’-O-β-D-glucosyl-5-O-methylvisamminol ameliorates imiquimod-induced psoriasis-like dermatitis and inhibits inflammatory cytokines production by suppressing the NF-κB and MAPK signaling pathways. Brazilian Journal of Medical and Biological Research. 2020; 53(12): e10109. doi: 10.1590/1414-431X202010109
- Rønholt K, Nielsen ALL, Johansen C, et al. IL-37 Expression Is Downregulated in Lesional Psoriasis Skin. ImmunoHorizons. 2020; 4(11): 754-761. doi: 10.4049/immunohorizons.2000083
- Zhao W, Xiao S, Li H, et al. MAPK Phosphatase-1 Deficiency Exacerbates the Severity of Imiquimod-Induced Psoriasiform Skin Disease. Frontiers in Immunology. 2018; 9. doi: 10.3389/fimmu.2018.00569
- He Q, Chen H, Li W, et al. IL-36 cytokine expression and its relationship with p38 MAPK and NF-κB pathways in psoriasis vulgaris skin lesions. Journal of Huazhong University of Science and Technology. 2013; 33(4): 594-599. doi: 10.1007/s11596-013-1164-1
- Matsumoto M, Tanaka T, Kaisho T, et al. A Novel LPS-Inducible C-Type Lectin Is a Transcriptional Target of NF-IL6 in Macrophages. The Journal of Immunology. 1999; 163(9): 5039-5048. doi: 10.4049/jimmunol.163.9.5039
- Tan R, Zhong X, Han R, et al. Macrophages mediate psoriasis via Mincle-dependent mechanism in mice. Cell Death Discovery. 2023; 9(1). doi: 10.1038/s41420-023-01444-8
- Liu Y, Chen J, Zhang Z, et al. NLRP3 inflammasome activation mediates radiation-induced pyroptosis in bone marrow-derived macrophages. Cell Death & Disease. 2017; 8(2): e2579-e2579. doi: 10.1038/cddis.2016.460
- Miglio G, Veglia E, Fantozzi R. Fumaric acid esters prevent the NLRP3 inflammasome-mediated and ATP-triggered pyroptosis of differentiated THP-1 cells. International Immunopharmacology. 2015; 28(1): 215-219. doi: 10.1016/j.intimp.2015.06.011
- Jo EK, Kim JK, Shin DM, et al. Molecular mechanisms regulating NLRP3 inflammasome activation. Cellular & Molecular Immunology. 2015; 13(2): 148-159. doi: 10.1038/cmi.2015.95
- Elliott EI, Sutterwala FS. Initiation and perpetuation of NLRP3 inflammasome activation and assembly. Immunological Reviews. 2015; 265(1): 35-52. doi: 10.1111/imr.12286
- Guo W, Liu W, Chen Z, et al. Tyrosine phosphatase SHP2 negatively regulates NLRP3 inflammasome activation via ANT1-dependent mitochondrial homeostasis. Nature Communications. 2017; 8(1). doi: 10.1038/s41467-017-02351-0
- Deng G, Chen W, Wang P, et al. Inhibition of NLRP3 inflammasome-mediated pyroptosis in macrophage by cycloastragenol contributes to amelioration of imiquimod-induced psoriasis-like skin inflammation in mice. International Immunopharmacology. 2019; 74: 105682. doi: 10.1016/j.intimp.2019.105682
- Syed SN, Weigert A, Brüne B. Sphingosine Kinases are Involved in Macrophage NLRP3 Inflammasome Transcriptional Induction. International Journal of Molecular Sciences. 2020; 21(13): 4733. doi: 10.3390/ijms21134733
- Gaire BP, Lee CH, Kim W, et al. Lysophosphatidic Acid Receptor 5 Contributes to Imiquimod-Induced Psoriasis-Like Lesions through NLRP3 Inflammasome Activation in Macrophages. Cells. 2020; 9(8): 1753. doi: 10.3390/cells9081753
- Balasubramanian S, Eckert R. Keratinocyte proliferation, differentiation, and apoptosis—Differential mechanisms of regulation by curcumin, EGCG and apigenin. Toxicology and Applied Pharmacology. 2007; 224(3): 214-219. doi: 10.1016/j.taap.2007.03.020
- Hsu S, Yamamoto T, Borke J, et al. Green Tea Polyphenol-Induced Epidermal Keratinocyte Differentiation Is Associated with Coordinated Expression of p57/KIP2 and Caspase 14. The Journal of Pharmacology and Experimental Therapeutics. 2005; 312(3): 884-890. doi: 10.1124/jpet.104.076075
- Chamcheu JC, Siddiqui IA, Adhami VM, et al. Chitosan-based nanoformulated (– )-epigallocatechin-3-gallate (EGCG) modulates human keratinocyte-induced responses and alleviates imiquimod-induced murine psoriasiform dermatitis. International Journal of Nanomedicine. 2018; 13: 4189-4206. doi: 10.2147/ijn.s165966
- Lee WR, Chou WL, Lin ZC, et al. Laser-assisted nanocarrier delivery to achieve cutaneous siRNA targeting for attenuating psoriasiform dermatitis. Journal of Controlled Release. 2022; 347: 590-606. doi: 10.1016/j.jconrel.2022.05.032
- Jiang Q, Wei B, You M, et al. d-mannose blocks the interaction between keratinocytes and Th17 cells to alleviate psoriasis by inhibiting HIF-1α/CCL20 in mice. International Immunopharmacology. 2023; 118: 110087. doi: 10.1016/j.intimp.2023.110087
- Szeto A, Sun-Suslow N, Mendez AJ, et al. Regulation of the macrophage oxytocin receptor in response to inflammation. American Journal of Physiology-Endocrinology and Metabolism. 2017; 312(3): E183-E189. doi: 10.1152/ajpendo.00346.2016
- Chiang CC, Cheng WJ, Korinek M, et al. Neutrophils in Psoriasis. Frontiers in Immunology. 2019; 10. doi: 10.3389/fimmu.2019.02376
- Hayakawa N, Noguchi M, Takeshita S, et al. Structure–activity relationship study, target identification, and pharmacological characterization of a small molecular IL-12/23 inhibitor, APY0201. Bioorganic & Medicinal Chemistry. 2014; 22(11): 3021-3029. doi: 10.1016/j.bmc.2014.03.036
- Oppmann B, Lesley R, Blom B, et al. Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity. 2000; 13(5): 715-725. doi: 10.1016/S1074-7613(00)00070-4
- Luu M, Binder K, Hartmann S, et al. Transcription factor c-Rel mediates communication between commensal bacteria and mucosal lymphocytes. Journal of Leukocyte Biology. 2021; 111(5): 1001-1007. doi: 10.1002/jlb.3ab0621-350r
- Chenoweth DM, Harki DA, Dervan PB. Solution-Phase Synthesis of Pyrrole−Imidazole Polyamides. Journal of the American Chemical Society. 2009; 131(20): 7175-7181. doi: 10.1021/ja901307m
- Armstrong AW, Read C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis. JAMA. 2020; 323(19): 1945. doi: 10.1001/jama.2020.4006
- Setten RL, Rossi JJ, Han S ping. The current state and future directions of RNAi-based therapeutics. Nature Reviews Drug Discovery. 2019; 18(6): 421-446. doi: 10.1038/s41573-019-0017-4
- Tong L, Zhao Q, Datan E, et al. Triptolide: reflections on two decades of research and prospects for the future. Natural Product Reports. 2020; 38(4): 843-860. doi: 10.1039/d0np00054j
- Silvestrini AVP, Garcia Praça F, Leite MN, et al. Liquid crystalline nanoparticles enable a multifunctional approach for topical psoriasis therapy by co-delivering triptolide and siRNAs. International Journal of Pharmaceutics. 2023; 640: 123019. doi: 10.1016/j.ijpharm.2023.123019
- Joseph SB, Castrillo A, Laffitte BA, et al. Reciprocal regulation of inflammation and lipid metabolism by liver X receptors. Nature Medicine. 2003; 9(2): 213-219. doi: 10.1038/nm820
- Gadde S, Even‐Or O, Kamaly N, et al. Development of Therapeutic Polymeric Nanoparticles for the Resolution of Inflammation. Advanced Healthcare Materials. 2014; 3(9): 1448-1456. doi: 10.1002/adhm.201300688
- Ng CY, Huang YH, Chu CF, et al. Risks for Staphylococcus aureus colonization in patients with psoriasis: a systematic review and meta-analysis. British Journal of Dermatology. 2017; 177(4): 967-977. doi: 10.1111/bjd.15366
- Boyles MSP, Kristl T, Andosch A, et al. Chitosan functionalisation of gold nanoparticles encourages particle uptake and induces cytotoxicity and pro-inflammatory conditions in phagocytic cells, as well as enhancing particle interactions with serum components. Journal of Nanobiotechnology. 2015; 13(1). doi: 10.1186/s12951-015-0146-9
- Yu X, Yi H, Guo C, et al. Pattern recognition scavenger receptor CD204 attenuates Toll-like receptor 4-induced NF-kappaB activation by directly inhibiting ubiquitination of tumor necrosis factor (TNF) receptor-associated factor 6. Journal of Biological Chemistry. 2011; 286(21): 18795-18806. doi: 10.1074/jbc.M111.224345
- Yi H, Xu X, Gao P, et al. Pattern recognition scavenger receptor SRA/CD204 down-regulates Toll-like receptor 4 signaling-dependent CD8 T-cell activation. Blood. 2009; 113(23): 5819-5828. doi: 10.1182/blood-2008-11-190033
- Ojewole JAO. Antinociceptive, anti-inflammatory and antidiabetic properties of Hypoxis hemerocallidea Fisch. & C.A. Mey. (Hypoxidaceae) corm [‘African Potato’] aqueous extract in mice and rats. Journal of Ethnopharmacology. 2006; 103(1): 126-134. doi: 10.1016/j.jep.2005.07.012
- Gautam A, Dixit S, Embers M, et al. Different Patterns of Expression and of IL-10 Modulation of Inflammatory Mediators from Macrophages of Lyme Disease-Resistant and-Susceptible Mice. Stevenson B, ed. PLoS ONE. 2012; 7(9): e43860. doi: 10.1371/journal.pone.0043860
- Kumar S, Shukla R, Ranjan P, et al. Interleukin-10: A Compelling Therapeutic Target in Patients With Irritable Bowel Syndrome. Clinical Therapeutics. 2017; 39(3): 632-643. doi: 10.1016/j.clinthera.2017.01.030
- Mahapatro A, Singh DK. Biodegradable nanoparticles are excellent vehicle for site directed in-vivo delivery of drugs and vaccines. Journal of Nanobiotechnology. 2011; 9(1): 55. doi: 10.1186/1477-3155-9-55
- Xiao RZ, Zeng ZW, Zhou GL, et al. Recent advances in PEG-PLA block copolymer nanoparticles. International Journal of Nanomedicine. 2010; 5: 1057-1065. doi: 10.2147/IJN.S14912
- Kim K, Yu M, Zong X, et al. Control of degradation rate and hydrophilicity in electrospun non-woven poly(D,L-lactide) nanofiber scaffolds for biomedical applications. Biomaterials. 2003; 24(27): 4977-4985. doi: 10.1016/S0142-9612(03)00407-1
- Duncan SA, Dixit S, Sahu R, et al. Prolonged Release and Functionality of Interleukin-10 Encapsulated within PLA-PEG Nanoparticles. Nanomaterials. 2019; 9(8): 1074. doi: 10.3390/nano9081074
- Rajendrakumar SK, Revuri V, Samidurai M, et al. Peroxidase-Mimicking Nanoassembly Mitigates Lipopolysaccharide-Induced Endotoxemia and Cognitive Damage in the Brain by Impeding Inflammatory Signaling in Macrophages. Nano Letters. 2018; 18(10): 6417-6426. doi: 10.1021/acs.nanolett.8b02785
- Chua RA, Arbiser JL, Chua RA, et al. The role of angiogenesis in the pathogenesis of psoriasis. Autoimmunity. 2009; 42(7): 574-579. doi: 10.1080/08916930903002461
- Young HS, Summers AM, Read IR, et al. Interaction between genetic control of vascular endothelial growth factor production and retinoid responsiveness in psoriasis. Journal of Investigative Dermatology. 2006; 126(2): 453-459. doi: 10.1038/sj.jid.5700096
- Xia YP, Li B, Hylton D, et al. Transgenic delivery of VEGF to mouse skin leads to an inflammatory condition resembling human psoriasis. Blood. 2003; 102(1): 161-168. doi: 10.1182/blood-2002-12-3793
- Schonthaler HB, Huggenberger R, Wculek SK, et al. Systemic anti-VEGF treatment strongly reduces skin inflammation in a mouse model of psoriasis. Proceedings of the National Academy of Sciences. 2009; 106(50): 21264-21269. doi: 10.1073/pnas.0907550106
- Roy B, Das A, Ashish K, et al. Neuropathy with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Neurology. 2019; 93(2). doi: 10.1212/wnl.0000000000007743
- Kunstfeld R, Hirakawa S, Hong YK, et al. Induction of cutaneous delayed-type hypersensitivity reactions in VEGF-A transgenic mice results in chronic skin inflammation associated with persistent lymphatic hyperplasia. Blood. 2004; 104(4): 1048-1057. doi: 10.1182/blood-2003-08-2964
- Hvid H, Teige I, Kvist PH, et al. TPA induction leads to a Th17-like response in transgenic K14/VEGF mice: a novel in vivo screening model of psoriasis. International Immunology. 2008; 20(8): 1097-1106. doi: 10.1093/intimm/dxn068
- Sun H, Zhao Y, Zhang P, et al. Transcutaneous delivery of mung bean-derived nanoparticles for amelioration of psoriasis-like skin inflammation. Nanoscale. 2022; 14(8): 3040-3048. doi: 10.1039/d1nr08229a
- Boldeiu A, Simion M, Mihalache I, et al. Comparative analysis of honey and citrate stabilized gold nanoparticles: In vitro interaction with proteins and toxicity studies. Journal of Photochemistry and Photobiology B: Biology. 2019; 197: 111519. doi: 10.1016/j.jphotobiol.2019.111519
- Erdogan MA, Erdogan A, Erbas O. The Anti-Seizure Effect of Liraglutide on Ptz-Induced Convulsions Through its Anti-Oxidant and Anti-Inflammatory Properties. Neurochemical Research. 2022; 48(1): 188-195. doi: 10.1007/s11064-022-03736-4
- Subramanian AP, John AA, Vellayappan MV, et al. Honey and its Phytochemicals: Plausible Agents in Combating Colon Cancer through its Diversified Actions. Journal of Food Biochemistry. 2016; 40(4): 613-629. doi: 10.1111/jfbc.12239
- Zhang L, Virgous C, Si H. Synergistic anti-inflammatory effects and mechanisms of combined phytochemicals. The Journal of Nutritional Biochemistry. 2019; 69: 19-30. doi: 10.1016/j.jnutbio.2019.03.009
- Navaei‐Alipour N, Mastali M, Ferns GA, et al. The effects of honey on pro‐ and anti‐inflammatory cytokines: A narrative review. Phytotherapy Research. 2021; 35(7): 3690-3701. doi: 10.1002/ptr.7066
- Cai SQ, Zhang Q, Zhao XH, et al. The In Vitro Anti-Inflammatory Activities of Galangin and Quercetin towards the LPS-Injured Rat Intestinal Epithelial (IEC-6) Cells as Affected by Heat Treatment. Molecules. 2021; 26(24): 7495. doi: 10.3390/molecules26247495
- Bharadwaj KK, Rabha B, Pati S, et al. Green Synthesis of Gold Nanoparticles Using Plant Extracts as Beneficial Prospect for Cancer Theranostics. Molecules. 2021; 26(21): 6389. doi: 10.3390/molecules26216389
- Jannathul Firdhouse M, Lalitha P. Biogenic Green Synthesis of Gold Nanoparticles and Their Applications – a Review of Promising Properties. SSRN; 2022.
- Duncan JBW, Basu S, Vivekanand P. Honey gold nanoparticles attenuate the secretion of IL-6 by LPS-activated macrophages. Sharma D, ed. PLOS ONE. 2023; 18(9): e0291076. doi: 10.1371/journal.pone.0291076
- Li Y, Liu Y, Fu Y, et al. The triggering of apoptosis in macrophages by pristine graphene through the MAPK and TGF-beta signaling pathways. Biomaterials. 2012; 33(2): 402-411. doi: 10.1016/j.biomaterials.2011.09.091
- Zhou H, Zhao K, Li W, et al. The interactions between pristine graphene and macrophages and the production of cytokines/chemokines via TLR- and NF-κB-related signaling pathways. Biomaterials. 2012; 33(29): 6933-6942. doi: 10.1016/j.biomaterials.2012.06.064
- Crisan D, Scharffetter‐Kochanek K, Crisan M, et al. Topical silver and gold nanoparticles complexed with Cornus mas suppress inflammation in human psoriasis plaques by inhibiting NF‐κB activity. Experimental Dermatology. 2018; 27(10): 1166-1169. doi: 10.1111/exd.13707
- Shukla R, Bansal V, Chaudhary M, et al. Biocompatibility of Gold Nanoparticles and Their Endocytotic Fate Inside the Cellular Compartment: A Microscopic Overview. Langmuir. 2005; 21(23): 10644-10654. doi: 10.1021/la0513712
- Chen T, Fu L, Guo Z, et al. Involvement of high mobility group box‐1 in imiquimod‐induced psoriasis‐like mice model. The Journal of Dermatology. 2016; 44(5): 573-581. doi: 10.1111/1346-8138.13695
- Jiang L, Shao Y, Tian Y, et al. Nuclear Alarmin Cytokines in Inflammation. Rao X, ed. Journal of Immunology Research. 2020; 2020: 1-8. doi: 10.1155/2020/7206451
- Kayagaki N, Kornfeld O, Lee B, et al. NINJ1 mediates plasma membrane rupture during lytic cell death. Nature. 2021; 591(7848): 131-136. doi: 10.1038/s41586-021-03218-7
- Matsui Y, Takemura N, Shirasaki Y, et al. Nanaomycin E inhibits NLRP3 inflammasome activation by preventing mitochondrial dysfunction. International Immunology. 2022; 34(10): 505-518. doi: 10.1093/intimm/dxac028
- Guarda G, Braun M, Staehli F, et al. Type I Interferon Inhibits Interleukin-1 Production and Inflammasome Activation. Immunity. 2011; 34(2): 213-223. doi: 10.1016/j.immuni.2011.02.006
- Shirasuna K, Usui F, Karasawa T, et al. Nanosilica-induced placental inflammation and pregnancy complications: different roles of the inflammasome components NLRP3 and ASC. Journal of Reproductive Immunology. 2014; 106: 14. doi: 10.1016/j.jri.2014.09.035
- Kanno S, Furuyama A, Hirano S. A Murine Scavenger Receptor MARCO Recognizes Polystyrene Nanoparticles. Toxicological Sciences. 2007; 97(2): 398-406. doi: 10.1093/toxsci/kfm050
- Mukhopadhyay S, Varin A, Chen Y, et al. SR-A/MARCO–mediated ligand delivery enhances intracellular TLR and NLR function, but ligand scavenging from cell surface limits TLR4 response to pathogens. Blood. 2011; 117(4): 1319-1328. doi: 10.1182/blood-2010-03-276733
- Hara K, Shirasuna K, Usui F, et al. Interferon-Tau Attenuates Uptake of Nanoparticles and Secretion of Interleukin-1β in Macrophages. Allen IC, ed. PLoS ONE. 2014; 9(12): e113974. doi: 10.1371/journal.pone.0113974
- Dhanashree S, Fish A, Debnath M, et al. Sprayable inflammasome-inhibiting lipid nanorods in a polymeric scaffold for psoriasis therapy. Nature Communications. 2024; 15(1): 9035. doi: 10.1038/s41467-024-53396-x
- Feng X, Liu D, Li Z, et al. Bioactive modulators targeting STING adaptor in cGAS-STING pathway. Drug Discovery Today. 2020; 25(1): 230-237. doi: 10.1016/j.drudis.2019.11.007
- Ebina M, Steinberg SM, Mulshine JL, et al. Relationship of p53 overexpression and up-regulation of proliferating cell nuclear antigen with the clinical course of non-small cell lung cancer. Cancer Research. 1994; 54(9): 2496-2503.
- Chan ESL, Cronstein BN. Methotrexate—how does it really work? Nature Reviews Rheumatology. 2010; 6(3): 175-178. doi: 10.1038/nrrheum.2010.5
- Xu J, Chen H, Chu Z, et al. A multifunctional composite hydrogel as an intrinsic and extrinsic coregulator for enhanced therapeutic efficacy for psoriasis. Journal of Nanobiotechnology. 2022; 20(1): 155. doi: 10.1186/s12951-022-01368-y
- Varol C, Mildner A, Jung S. Macrophages: Development and Tissue Specialization. Annual Review of Immunology. 2015; 33(1): 643-675. doi: 10.1146/annurev-immunol-032414-112220
- Jiang D, Liang J, Noble PW. Hyaluronan as an Immune Regulator in Human Diseases. Physiological Reviews. 2011; 91(1): 221-264. doi: 10.1152/physrev.00052.2009
- Duncan R. The dawning era of polymer therapeutics. Nature Reviews Drug Discovery. 2003; 2(5): 347-360. doi: 10.1038/nrd1088
- Zhu Y, Crewe C, Scherer PE. Hyaluronan in adipose tissue: Beyond dermal filler and therapeutic carrier. Science Translational Medicine. 2016; 8(323). doi: 10.1126/scitranslmed.aad6793
- Rao NV, Yoon HY, Han HS, et al. Recent developments in hyaluronic acid-based nanomedicine for targeted cancer treatment. Expert Opinion on Drug Delivery. 2015; 13(2): 239-252. doi: 10.1517/17425247.2016.1112374
- Jiang D, Liang J, Fan J, et al. Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nature Medicine. 2005; 11(11): 1173-1179. doi: 10.1038/nm1315
- Zheng L, Riehl TE, Stenson WF. Regulation of Colonic Epithelial Repair in Mice by Toll-Like Receptors and Hyaluronic Acid. Gastroenterology. 2009; 137(6): 2041-2051. doi: 10.1053/j.gastro.2009.08.055
- Mummert ME, Mohamadzadeh M, Mummert DI, et al. Development of a Peptide Inhibitor of Hyaluronan-Mediated Leukocyte Trafficking. The Journal of Experimental Medicine. 2000; 192(6): 769-780. doi: 10.1084/jem.192.6.769
- Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013; 496(7446): 445-455. doi: 10.1038/nature12034
- Lee WH, Rho JG, Yang Y, et al. Hyaluronic Acid Nanoparticles as a Topical Agent for Treating Psoriasis. ACS Nano. 2022; 16(12): 20057-20074. doi: 10.1021/acsnano.2c07843
- Sendão RMS, Crista DMA, Afonso ACP, et al. Insight into the hybrid luminescence showed by carbon dots and molecular fluorophores in solution. Physical Chemistry Chemical Physics. 2019; 21(37): 20919-20926. doi: 10.1039/c9cp03730f
- Kaur N, Mehta A, Mishra A, et al. Amphiphilic carbon dots derived by cationic surfactant for selective and sensitive detection of metal ions. Materials Science and Engineering: C. 2019; 95: 72-77. doi: 10.1016/j.msec.2018.10.058
- Tan M, Zhang L, Tang R, et al. Enhanced photoluminescence and characterization of multicolor carbon dots using plant soot as a carbon source. Talanta. 2013; 115: 950-956. doi: 10.1016/j.talanta.2013.06.061
- Imler TJ, Petro TM. Decreased severity of experimental autoimmune encephalomyelitis during resveratrol administration is associated with increased IL-17+IL-10+ T cells, CD4− IFN-γ+ cells, and decreased macrophage IL-6 expression. International Immunopharmacology. 2009; 9(1): 134-143. doi: 10.1016/j.intimp.2008.10.015
- Mikita J, Dubourdieu-Cassagno N, Deloire MS, et al. Altered M1/M2 activation patterns of monocytes in severe relapsing experimental rat model of multiple sclerosis. Amelioration of clinical status by M2 activated monocyte administration. Multiple Sclerosis Journal. 2010; 17(1): 2-15. doi: 10.1177/1352458510379243
- Platt AM, Mowat AMcI. Mucosal macrophages and the regulation of immune responses in the intestine. Immunology Letters. 2008; 119(1-2): 22-31. doi: 10.1016/j.imlet.2008.05.009
- Qualls JE, Kaplan AM, Van Rooijen N, et al. Suppression of experimental colitis by intestinal mononuclear phagocytes. Journal of Leukocyte Biology. 2006; 80(4): 802-815. doi: 10.1189/jlb.1205734
- Schappe MS, Szteyn K, Stremska ME, et al. Chanzyme TRPM7 Mediates the Ca2+ Influx Essential for Lipopolysaccharide-Induced Toll-Like Receptor 4 Endocytosis and Macrophage Activation. Immunity. 2018; 48(1): 59-74.e5. doi: 10.1016/j.immuni.2017.11.026
- Tedesco S, Scattolini V, Albiero M, et al. Mitochondrial Calcium Uptake Is Instrumental to Alternative Macrophage Polarization and Phagocytic Activity. International Journal of Molecular Sciences. 2019; 20(19): 4966. doi: 10.3390/ijms20194966
- Feng N, Liang L, Fan M, et al. Treating Autoimmune Inflammatory Diseases with an siERN1-Nanoprodrug That Mediates Macrophage Polarization and Blocks Toll-like Receptor Signaling. ACS Nano. 2021; 15(10): 15874-15891. doi: 10.1021/acsnano.1c03726
- Zhao ZQ, Chen BZ, Gan JL, et al. Dual-functional microneedle with programmatic regulation of macrophage for autoimmune psoriasis treatment. Nano Research. 2024; 17(8): 7436-7448. doi: 10.1007/s12274-024-6711-5
- Iuliano M, Grimaldi L, Rosa P, et al. Extracellular vescicles in psoriasis: from pathogenesis to possible roles in therapy. Frontiers in Immunology. 2024; 15. doi: 10.3389/fimmu.2024.1360618
- Han C, Fu YX. β-Catenin regulates tumor-derived PD-L1. Journal of Experimental Medicine. 2020; 217(11). doi: 10.1084/jem.20200684
- Wang Z, Qin Z, Wang J, et al. Engineering extracellular vesicles with macrophage membrane fusion for ameliorating imiquimod-induced psoriatic skin inflammation. Journal of Dermatological Treatment. 2023; 34(1). doi: 10.1080/09546634.2023.2220445
- Jun L, Yuan Z, Shi S, et al. Microneedle patches incorporating zinc-doped mesoporous silica nanoparticles loaded with betamethasone dipropionate for psoriasis treatment. Journal of Nanobiotechnology. 2024; 22.
- Ho Y, Chang Y, Yeh C. Improving Nanoparticle Penetration in Tumors by Vascular Disruption with Acoustic Droplet Vaporization. Theranostics. 2016; 6(3): 392-403. doi: 10.7150/thno.13727
- Soto F, Jeerapan I, Silva‐López C, et al. Noninvasive Transdermal Delivery System of Lidocaine Using an Acoustic Droplet‐Vaporization Based Wearable Patch. Small. 2018; 14(49). doi: 10.1002/smll.201803266
- Xi L, Han Y, Liu C, et al. Sonodynamic therapy by phase-transition nanodroplets for reducing epidermal hyperplasia in psoriasis. Journal of Controlled Release. 2022; 350: 435-447. doi: 10.1016/j.jconrel.2022.08.038
- Ambarus C, Yeremenko N, Tak PP, et al. Pathogenesis of spondyloarthritis. Current Opinion in Rheumatology. 2012; 24(4): 351-358. doi: 10.1097/bor.0b013e3283534df4
- Lubberts E. The IL-23–IL-17 axis in inflammatory arthritis. Nature Reviews Rheumatology. 2015; 11(7): 415-429. doi: 10.1038/nrrheum.2015.53
- EJNMMI Radiopharmacy and Chemistry. Abstracts from the 20th European symposium on radiopharmacy and radiopharmaceuticals. EJNMMI Radiopharmacy and Chemistry. 2023; 8(Suppl 1): 11.
- Fruchon S, Mouriot S, Thiollier T, et al. Repeated intravenous injections in non-human primates demonstrate preclinical safety of an anti-inflammatory phosphorus-based dendrimer. Nanotoxicology. 2014; 9(4): 433-441. doi: 10.3109/17435390.2014.940406
- Erol İ, Üstündağ Okur N, Orak D, et al. Tazarotene-loadedin situgels for potential management of psoriasis: biocompatibility, anti-inflammatory and analgesic effect. Pharmaceutical Development and Technology. 2020; 25(8): 909-918. doi: 10.1080/10837450.2020.1765180
- Danquah W, Meyer-Schwesinger C, Rissiek B, et al. Nanobodies that block gating of the P2X7 ion channel ameliorate inflammation. Science Translational Medicine. 2016; 8(366). doi: 10.1126/scitranslmed.aaf8463
Supporting Agencies
Copyright (c) 2025 Author(s)
License URL: https://creativecommons.org/licenses/by/4.0/

This site is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0).

Medical Genetics, University of Torino Medical School, Italy

Department of Biomedical, Surgical and Dental Sciences, University of Milan, Italy

